Survival rates for breast cancer patients with brain metastasis treated with radiation
Martin Kjær Simonsen,
Denmark
PO-1189
Abstract
Survival rates for breast cancer patients with brain metastasis treated with radiation
Authors: Martin Simonsen1, Birgitte Vrou Offersen2, Anders Bonde Jensen2
1Aarhus University Hospital , Department of Oncology, Aarhus, Denmark; 2Aarhus University Hospital, Department of Oncology, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Due to advancements in systemic treatment, the survival
of breast cancer (BC) patients (pts) has improved, resulting in an increased
incidence of brain metastases (BM). Treatment options for BM are limited and primarily
consist of palliative surgery and/or radiotherapy (RT)
Our aim is to analyze survival time for BC pts treated with RT either
alone or in combination with surgery, after first event of BM. Secondly, to
evaluate prognostic impact of predefined factors.
Material and Methods
Pts were identified retrospectively at a single
institutionand included if they
were treated with RT for their first event of BM between Jan 2015 and June 2020.
Statistics included Kaplan-Meier analysis and Log-rank test to evaluate
survival, and Chi-square tests to analyze impact of eventual prognostic
factors. The study was approved by the institutional research board.
Results
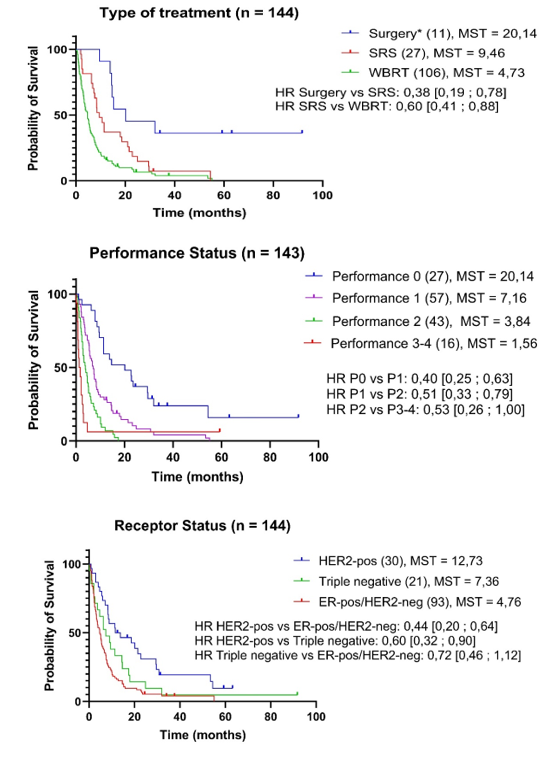
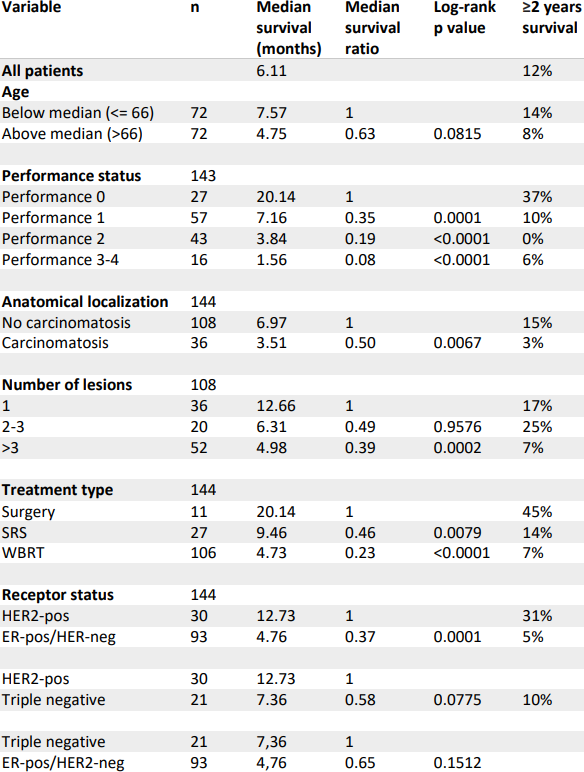
In total, 144 pts
were identified, of whom 106 (73.6%) and 27 (18.8%) received whole brain RT
(WBRT) and stereotactic radiosurgery (SRS), respectively. Eleven pts (7.6%)
underwent surgery followed by WBRT or SRS. A total of 129 pts (89.6%) had
extracranial metastatic disease at BM debut. Median overall survival (OS) was
6.1 months (mth). OS was shorter in the WBRT group (4.7 mth) than in the SRS
(9.5 mth) and surgery group (20.1 mth). Meningeal carcinomatosis (MC) led to
short OS (3.5 mth vs 7 mth for those without). OS depending on
performance status (PS) 0, 1, 2 and 3-4 was 20.1, 7.2, 3.8 and 1.6 mth,
respectively. OS for pts with 1, 2-3 or >3 brain metastases was 12.7, 6.3,
and 5 mth, respectively. Three molecular subgroups were defined (ER+/HER2-,
triple-negative, and HER2+ regardless ER) with corresponding OS 4.8, 7.4, and
12.7 mth. Pts in the ER+/HER2- group were older, had metastatic disease for a
longer time at BM, poorer PS, and were more likely to develop MC. Pts with BM
as first metastatic event had an OS of 20.1 mth, while pts who had received 1,
2-3 or >3 preceding treatment lines at BM debut had an OS of 4.9, 5.4, and
5.2 mth respectively.
Conclusion
Despite advancements
in the treatment of metastatic breast cancer, BM is associated with a poor
prognosis. PS, MC, metastatic burden, BC subtype, and number of systemic
treatment lines before BM influenced survival. These factors should be
considered when deciding treatment for pts with BM.