Outcome of male breast cancer patients at an academic university hospital in India
PO-1178
Abstract
Outcome of male breast cancer patients at an academic university hospital in India
Authors: Deep Chakrabarti1, Arunima Ghosh1, Mranalini Verma1, Divya Kukreja1, Naseem Akhtar2, Shiv Rajan2, Sumaira Qayoom3, Pooja Ramakant4, Vijay Kumar2, Kirti Srivastava1, Rajeev Gupta1, Madan Lal Bhatt1
1King George's Medical University, Radiotherapy, Lucknow, India; 2King George's Medical University, Surgical Oncology, Lucknow, India; 3King George's Medical University, Pathology, Lucknow, India; 4King George's Medical University, Endocrine Surgery, Lucknow, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Male breast cancer is a rare disease accounting for less than 1 % of all breast cancer cases worldwide. Most of our knowledge about them is based on retrospective datasets.
Material and Methods
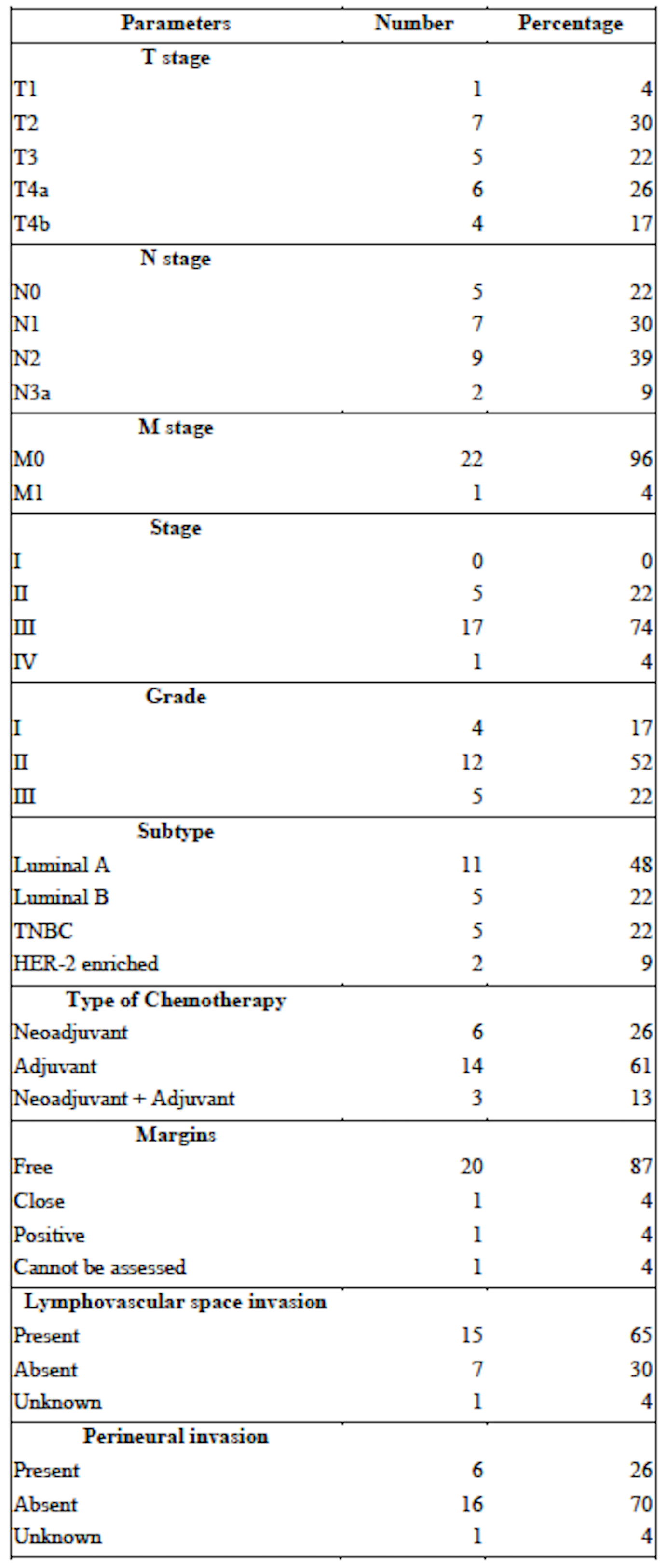
This retrospective cohort study included all patients of invasive male breast cancer treated at the radiotherapy department of a tertiary care academic university hospital in India between 2012 and 2020. Records were identified from a prospectively maintained database. Clinicopathological parameters, treatment details, recurrence patterns, and survival were determined.
Results
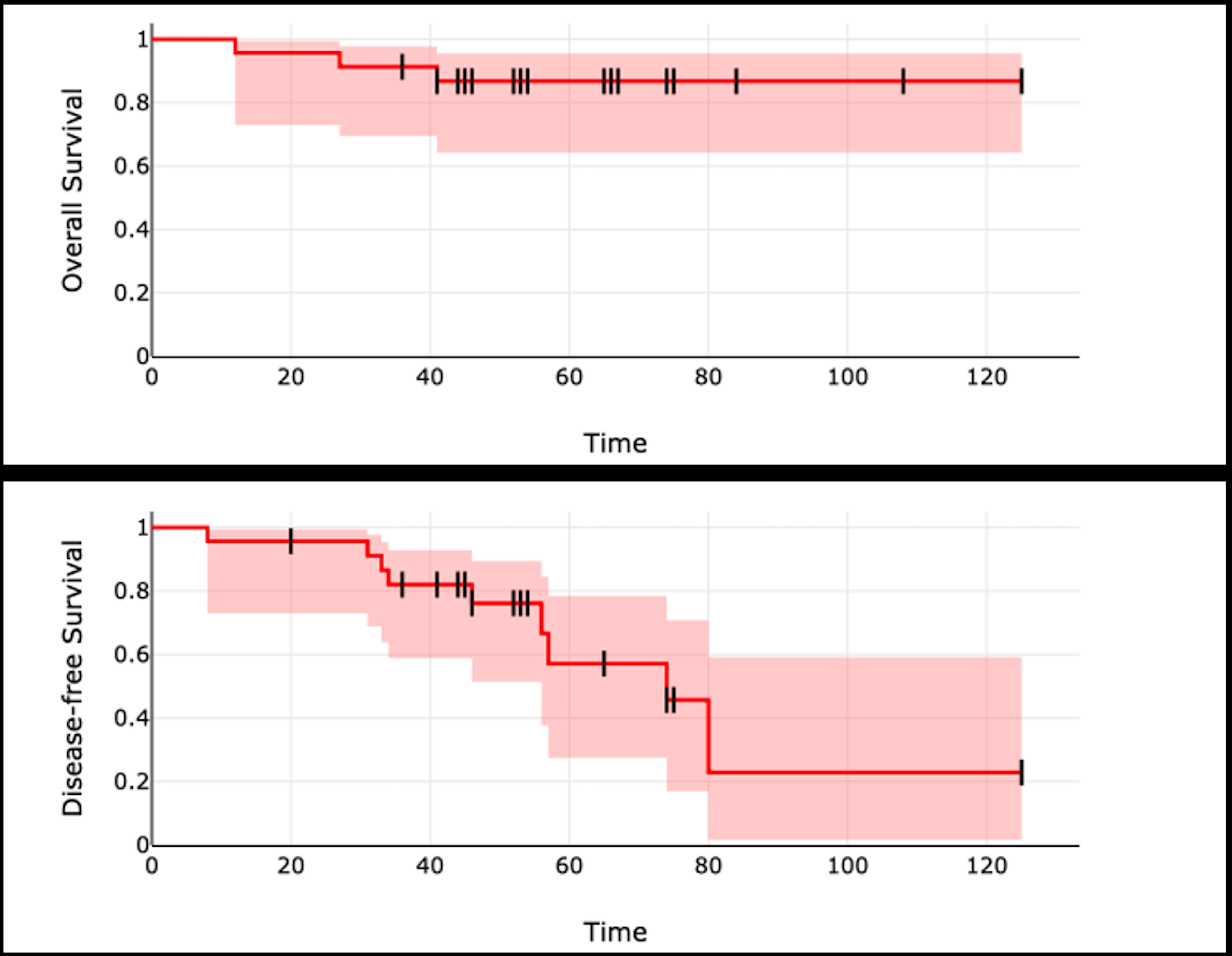
Twenty-three patients were included. The median age was 55 years. Most patients were UICC TNM composite stage III (74%) and node-positive (78%) with Scarff-Bloom-Richardson grade II (52%). One patient presented with metastatic disease upfront. Sixteen patients (70%) were estrogen receptor (ER) positive. Lymphovascular space invasion (LVSI) and perineural invasion (PNI) were present in 65% and 26% of patients respectively. The most common chemotherapy timing was adjuvant (61%), and the most commonly used regimen consisted of a triplet of 5-fluorouracil, an anthracycline (doxorubicin or epirubicin), and cyclophosphamide (FAC or FEC, 57%). Twenty-two patients underwent surgery (two lumpectomies, one wide local excision, 17 mastectomies) and subsequent radiotherapy to a dose of 42.6 Gy in 16 fractions. At a median follow up of 53 months (95% CI 47-67 months), three patients had died. Nine patients had local or distant failures (four bone metastases, one lung metastasis, four locoregional recurrences). The five-year disease-free survival (DFS) was 57%, and five-year overall survival (OS) was 87%.
Conclusion
Our reported cohort shows that most male breast cancer patients present with advanced stages, and most are node-positive with a high incidence of ER-positive disease and LVSI. Even with a relatively high incidence of bone metastasis, good five-year DFS, and OS are expected.