Comprehensive comparison of prognostic scores for patients with newly diagnosed brain metastases
PO-1157
Abstract
Comprehensive comparison of prognostic scores for patients with newly diagnosed brain metastases
Authors: Johannes Kraft1,2, Janita E. van Timmeren2, Simon Frei2, Michael Mayinger2, Kim Borsky2, Corinna Kirchner3,2, Luisa Sabrina Stark2, Stephanie Tanadini-Lang2, Fabian Wolpert4, Michael Weller4, Matthias Guckenberger2, Nicolaus Andratschke2
1University Hospital Würzburg, Department of Radiation-Oncology, Würzburg, Germany; 2University Hospital Zurich, Department of Radiation-Oncology, Zurich, Switzerland; 3Marienhospital Stuttgart, Department of Radiation-Oncology, Stuttgart, Germany; 4University Hospital Zurich, Department of Neurology, Zurich, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Numerous prognostic scores for assessment of patients' overall survival after the diagnosis of brain metastases have been developed in the last decades. Since the introduction of the first prognostic scores, overall survival of patients has dramatically changed, and it is unclear whether existing older scores are still relevant and can still compete with newer scores. The aim of our work is to provide a comprehensive overview and performance comparison of existing scores for brain metastases in a modern patient collective treated with upfront stereotactic radiosurgery for newly diagnosed brain metastases.
Material and Methods
Overall seventeen previously published prognostic scores were included for the comparison and were calculated for 470 patients receiving upfront stereotactic radiosurgery between 2014 and 2020. Prognostic scores were evaluated and ranked based on restricted mean survival time (RMST) and partial likelihood. Univariable and multivariable analysis were used to identify prognostic factors for OS. In addition, a score solely based on the assessment of the performance status was calculated and included in the performance comparison.
Results
The median OS of the cohort was 15.8 months (95% C.I.: 13.4‐20.1) Prognostic scores solely based on clinical parameters could be calculated for all patients (n=470). For 310 patients with a complete dataset of laboratory parameters, five additional laboratory scores could be calculated and were included in a separate overall ranking. When considering the entire cohort, GGS, the WBRT Score of Rades et al., RPA and a score based solely on the assessment of performance status showed the highest partial likelihood. In the evaluation of 310 patients with complete laboratory dataset and with inclusion of the laboratory scores, EC-GPA, LabBM, ECS, and the modified Glasgow Score displaced all the previously mentioned ones. RPA showed the largest between-group differences in terms of RMST. Multivariate analysis revealed laboratory parameters (hemoglobine, albumin, LDH and C-reactive protein) and performance status as the most significant parameters associated with OS.
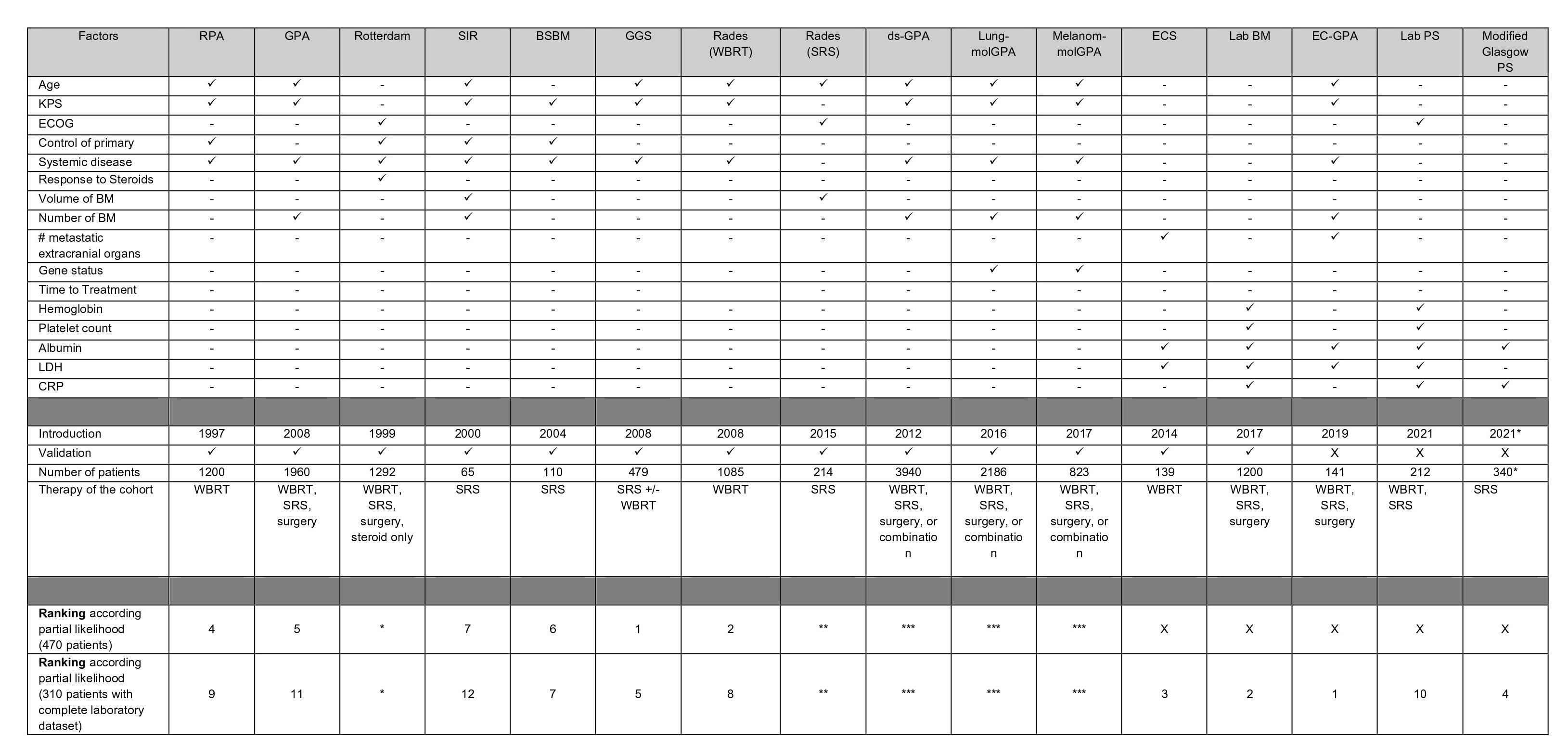
Table 1 - Overview of prognostic scores and ranking based on partial likelihood
not incorporated into the final comparison: *(treatment with corticosteroids), **(two subgroups), ***(evaluated in histology-specific subgroups)
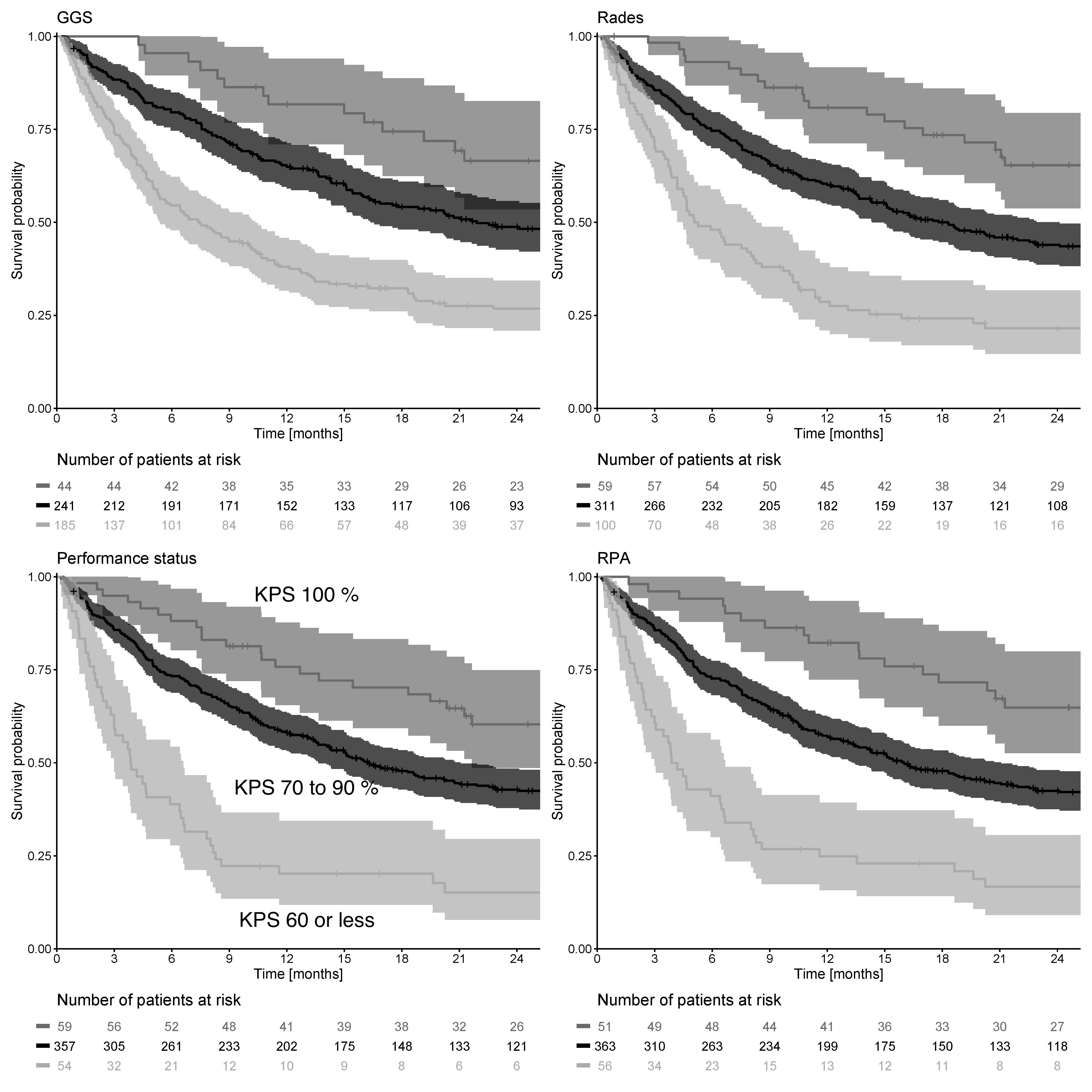
Figure 1 - 3-tiered Prognostic Scores achieving the highest partial likelihood within the entire cohort; Calculation of the Performance Status Score (see within Performance Status Score lower left)
Conclusion
Although recent scores incorporating laboratory parameters show the best performance in predicting overall survival, scores relying on clinical parameters only are still valid and appealing as they are easier to calculate and as the difference in overall performance is negligible. A score based only on performance status shows an excellent overall performance and thus is favored for universal use of a BM score for decision-making.