Survival after stereotactic radiosurgery for brain metastases – A single-institution experience
PO-1140
Abstract
Survival after stereotactic radiosurgery for brain metastases – A single-institution experience
Authors: Agon Olloni1,2, Olfred Hansen3,2, Charlotte Kristiansen4, Linda Edvardsson5, Morten Nielsen6, Stefan Starup Jeppesen7,2, Tine Schytte7,2
1Odense University Hospital , Department of Oncology , Odense , Denmark; 2University of Southern Denmark , Department of Clinical Research, Odense , Denmark; 3Odense University Hospital , Department of Oncology, Odense, Denmark; 4University Hospital of Southern Denmark, Lillebaelt Hospital, Department of Oncology, Vejle , Denmark; 5Kalmar County Hospital, Department of Oncology, Kalmar, Sweden; 6Odense University Hospital, Laboratory of Radiation Physics, Department of Oncology, Odense , Denmark; 7Odense University Hospital, Department of Oncology, Odense , Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Improved overall survival (OS)
due to advances in cancer treatment and improvements in neuroimaging results in
an increasing number of patients presenting with brain metastases.
Stereotactic radiosurgery
(SRS) is increasingly used instead of whole-brain radiotherapy (WBRT) for
patients with limited brain metastases, as WBRT has known side effects, which
are of increasing concern due to improvement in prognosis. The benefits of SRS
compared to WBRT include reduced toxicity, as it is possible to reduce the
radiation dose to the whole brain and an expected increase in local control.
However, despite treatment advances, the prognosis for the majority of patients
with brain metastases remains poor. This study aimed to evaluate survival after
the first treatment with SRS and identify groups of patients with a better
prognosis.
Material and Methods
Patients from a single institution with up to four
brain metastases, diameter <3 cm, treated from April 2011 to February 2018
were included, regardless of the primary cancer diagnosis. Single
metastases between 3 and 4 cm were allowed. Patients were prospectively
registered, and clinical data were gathered retrospectively (tumor histology,
performance status (PS), age, and number of metastases). As follow-up
procedure, MRI was performed one month after treatment and every 3rd month
hereafter. In case of progression or recurrence, the possibility of SRS, WBRT,
surgery, systemic treatment, or best supportive care was evaluated. No patients
were lost to follow up. The dose to the edge of the gross tumor volume (GTV)
was 20 Gy/ 1 F or, in case of larger metastases or proximity to organs at risk,
27 Gy/ 3F. All patients were planned with CT- and MR scans.
Radiologists and oncologists in collaboration defined GTV. The treatment was
performed with three arcs on a linac, one coplanar and two non-coplanar. Orfit®
5-points immobilization system was used. PTV margin was 2-3 mm.
Results
In total, 285 patients were treated with SRS. Baseline
characteristics in table 1. The median survival was eight months. OS after 1
and 2 years was 29% and 13% respectively. Median survival for breast cancer
patients was 19.4 months, 9.8 months for malignant melanoma, and 7.6 months for
lung cancer patients. Patients with a PS 0-1 and breast cancer diagnosis had
significantly better survival. Patients with PS ≥2 had a median survival
of only four months (table 2).
In a cox regression analysis PS, female sex and breast
cancer diagnosis had a statistically significant positive impact on survival,
whereas number of brain metastases (1 vs ≥2) and age ≤70 did not.
Conclusion
Compared to WBRT(historical data), SRS performed with VMAT appear to improve survival. The majority of the patients with brain metastases still have a poor prognosis, but selected patients gained improved survival. Patients with PS ≥2 have doubtful gain of SRS in terms of survival, but SRS may be effective as treatment of symptoms.
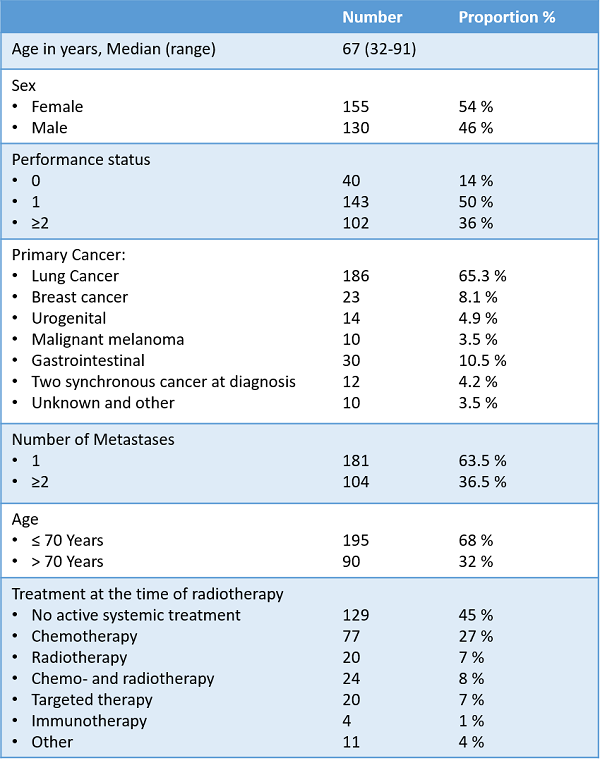
Table 1 Baseline Characteristics
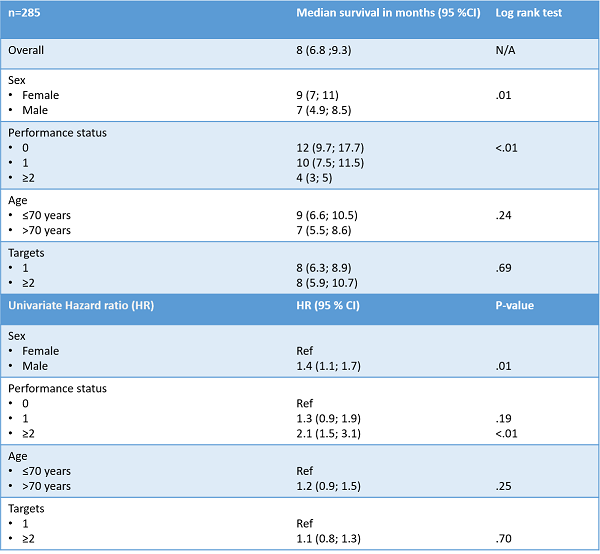
Table 2 Median survival and Hazard Ratios