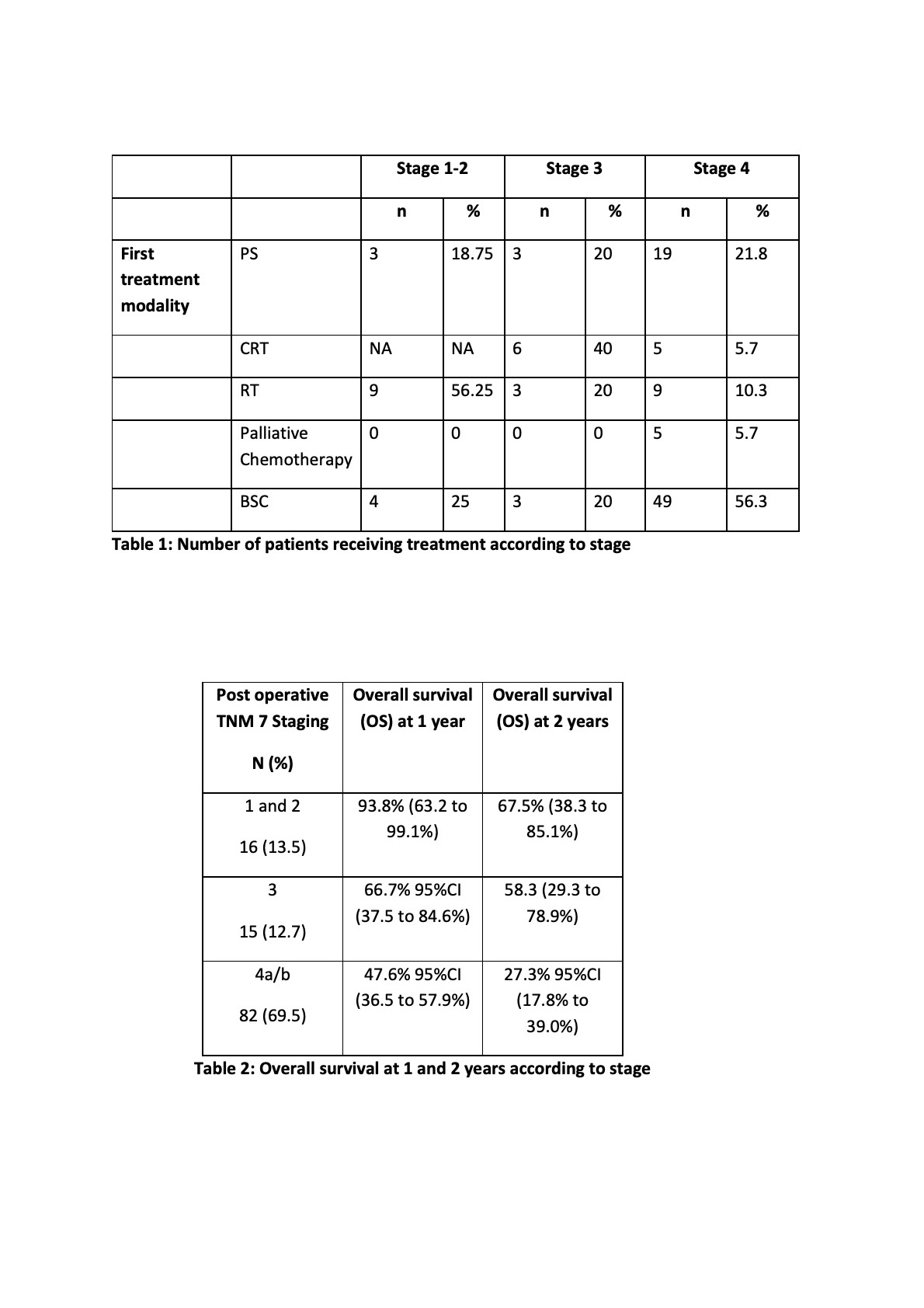
118 patients were evaluable. 35.6% were aged >70 and 33.1% were PS 2+. 26.3% patients had a prior cancer diagnosis, with 16% having a previous H&N cancer. PET-CT was performed in 11.5% of the T4 patients. 5 (4.24%) were upstaged post-operatively.
For stage 1-2 patients, primary surgery (PS) had a 100% overall survival (OS) at 2 years compared with radiotherapy (RT) alone (64.8%, CI 25.3-87.2).
For stage 3 patients, PS +/- adjuvant RT had a 1 year OS of 100% compared with primary chemoradiotherapy (CRT) (83.3%, CI 27.3-97.5) and RT alone (66.7%, 5.4-94.5). However, the 2 year OS rate for PS alone was 0%, whereas PS and adjuvant RT and CRT remained at 100% and 83.3% respectively.
For stage 4a/b patients, the 2yr OS with PS and adjuvant RT, PS alone, CRT and RT alone was 100%, 50% (20.8-73.6), 0% and 53.3% (12.5-82.7) respectively. Palliative platinum-based chemotherapy had a 2 year OS of 40% (5.2-75.3).
Of note, over 50% of patients received best supportive care (BSC).
The most common site of recurrence was at the primary site. Initial treatment modality did not appear to affect this.