Predicting radiation-induced neurocognitive decline in patients with brain or head & neck tumor
Fariba Tohidinezhad,
The Netherlands
PO-1108
Abstract
Predicting radiation-induced neurocognitive decline in patients with brain or head & neck tumor
Authors: Fariba Tohidinezhad1, Dario Di Perri1, Catharina M.L. Zegers1, Andre Dekker1, Wouter Van Elmpt1, Daniëlle Eekers1, Alberto Traverso1
1Maastricht University Medical Center, Department of Radiation Oncology (Maastro Clinic, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Irradiating brain or head & neck tumor with
curative or prophylactic intent, results in dose to the healthy surrounding
brain possibly resulting is clinical relevant side effects like neurocognitive
decline. Preservation of neurocognitive function is of paramount importance to maintain
the quality of life of the treated patients. Prediction models have the
potential to identify patients at high risk of developing radiation-induced
neurocognitive burden. This study summarizes and evaluates available prediction
models for estimating the risk of neurocognitive decline after cranial
irradiation.
Material and Methods
MEDLINE was searched on 4 March 2021 for
publications containing relevant truncation and MeSH terms related to “radiotherapy”,
“brain”, “prediction model”, and “neurocognitive impairments” (e.g., memory
dysfunction, learning and attention deficits, problem-solving incompetence, psychological
disorders). Two independent reviewers excluded studies according the following
criteria: lack of model specifications, no predictor in multivariate analysis,
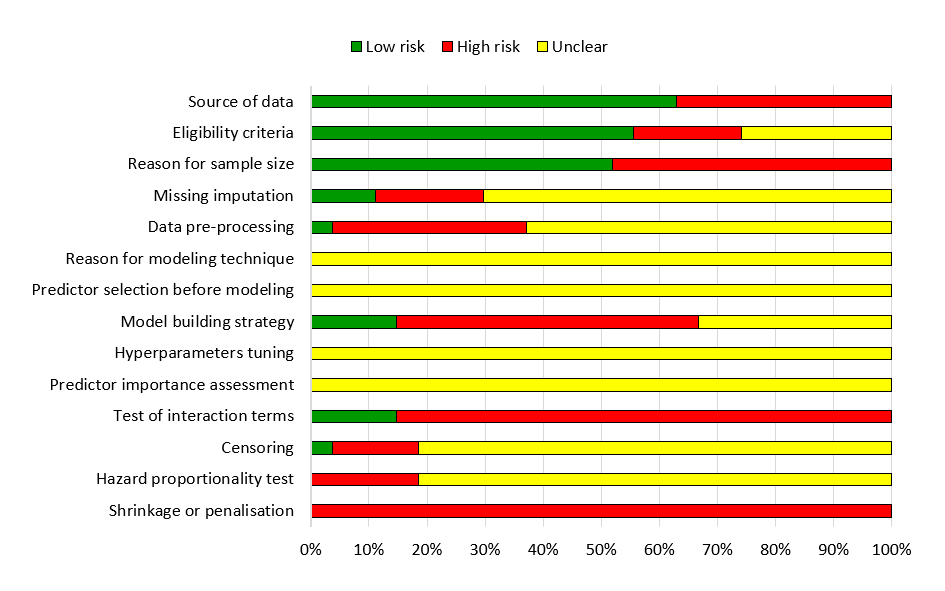
or no adult population. Quality of prediction models was assessed using 14 common
methodological considerations in machine learning proposed by Andaur Navarro CL et
al. (PMID: 33177137), including data source, data preparation, hyper-parameter
tuning, model building strategy, test of interaction terms, and applying
shrinkage or penalization methods.
Results
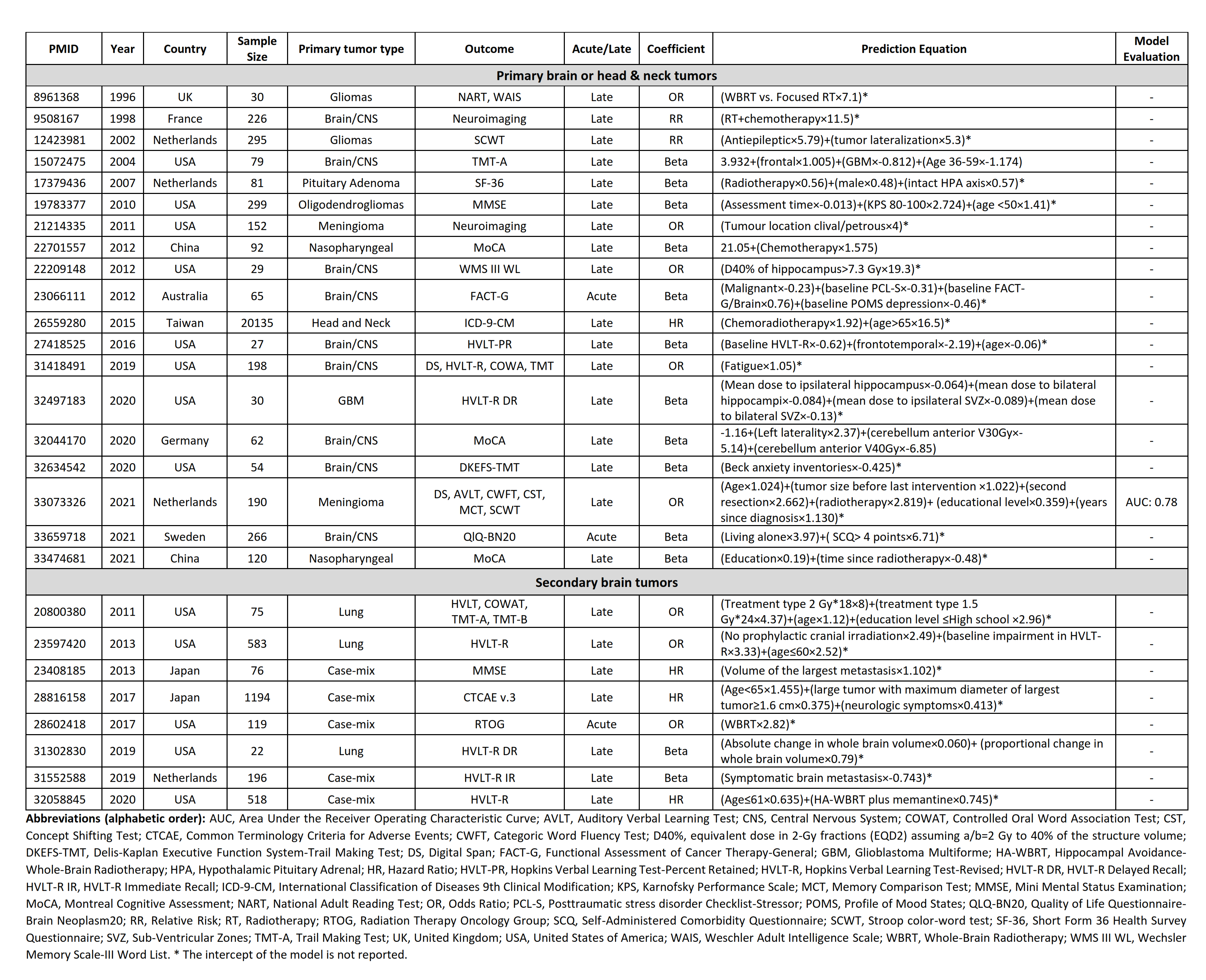
Of 3,351 studies reviewed, 27 studies met the pre-defined
eligibility criteria. Included studies were published between 1996 and 2021
with a median sample size of 119 and 55.6% male patients. Nineteen studies developed
a prediction model for patients with primary brain or head & neck tumors
and eight studies included patients with metastatic brain tumors. Four studies assessed
the effect of prophylactic cranial irradiation. Hopkins Verbal Learning Test-Revised
(n=7, 26%), Montreal Cognitive Assessment (n=3, 12%), and Mini Mental State
Examination (n=2, 7%) were the most frequent neurocognitive outcome assessment
tools. All studies used regression (n=14 linear, n=8 logistic, and n=5 cox
proportional hazard) as the machine learning method. Further details of the
included studies are described in Table 1. The median quality score was 2 out
of 14 and only one study assessed the area under the receiver operating
characteristic curve (Figure 1).
Conclusion
Clinical prediction models may support the risk
estimation of neurocognitive decline after brain radiotherapy, but existing
models have limited quality and are at high risk of bias. Therefore current
prediction models are of limited clinical value. Future studies should adhere
to model building standards and conduct model validation to derive a reliable
prediction model that can be used in clinical routine for decision support.