pre-treatment salivary flow predicts recovery of salivary flow after IMRT for head and neck cancer
PO-1095
Abstract
pre-treatment salivary flow predicts recovery of salivary flow after IMRT for head and neck cancer
Authors: Shinya Hiraoka1, Aya Nakajima1, Michio Yoshimura1, Takashi Mizowaki1
1Graduate School of Medicine, Kyoto University, Department of Radiation Oncology and Image-Applied Therapy, Kyoto, Japan
Show Affiliations
Hide Affiliations
Purpose or Objective
Xerostomia is one of the most significant adverse
events caused by radiotherapy and severely reduces patients' quality of life
for a lengthy period in patients with head and neck cancer. Intensity-modulated radiation therapy (IMRT) reduces the
incidence of xerostomia compared to conventional radiotherapy. However, most
patients experience temporary severe xerostomia, which requires several years
to recover, and limited reports indicate individual differences in the recovery
time. The purpose of this study was to evaluate the salivary recovery time and
rate after IMRT for head and neck cancer.
Material and Methods
In this study, we evaluated 57 patients with head
and neck cancer who received IMRT for curative intent and stimulated salivary
flow measurement between Jan 2012 and Dec 2018 at our institution. Xerostomia was
graded with the CTCAE v.4.0. The salivary recovery time was defined as when salivary
flow recovered beyond the mean salivary recovery rate after radiotherapy. The salivary
recovery rate was defined as "(the third quartile of salivary flow after
radiotherapy) / (pre-treatment salivary flow)." Patients were divided into
two groups for each explanatory variable; mean parotid glands dose, mean oral cavity
dose, pre-treatment salivary flow, age, sex, and chemotherapy status. The
salivary recovery time was compared using Cox proportional hazard model, and the
cumulative salivary recovery rate was estimated using the Kaplan-Meier method. The
salivary recovery rate was analyzed using the t-test and multiple regression
analysis. To evaluate the relevance between the salivary recovery rate and the
subjective symptoms, the difference in salivary recovery rate between each
xerostomia grade was analyzed using a one-way analysis of variance. P
values < 0.05 were considered statistically significant.
Results
The median follow-up period of salivary flow was 48
months, and the median salivary recovery rate was 58.2%. The median salivary
recovery time and the cumulative recovery rate at four years were 48 months and
52.9% in the high pre-treatment salivary flow group, whereas 18 months and 79.6%
in the low pre-treatment salivary flow group (P =
0.026). The mean parotid glands and oral dose were insignificant in the salivary
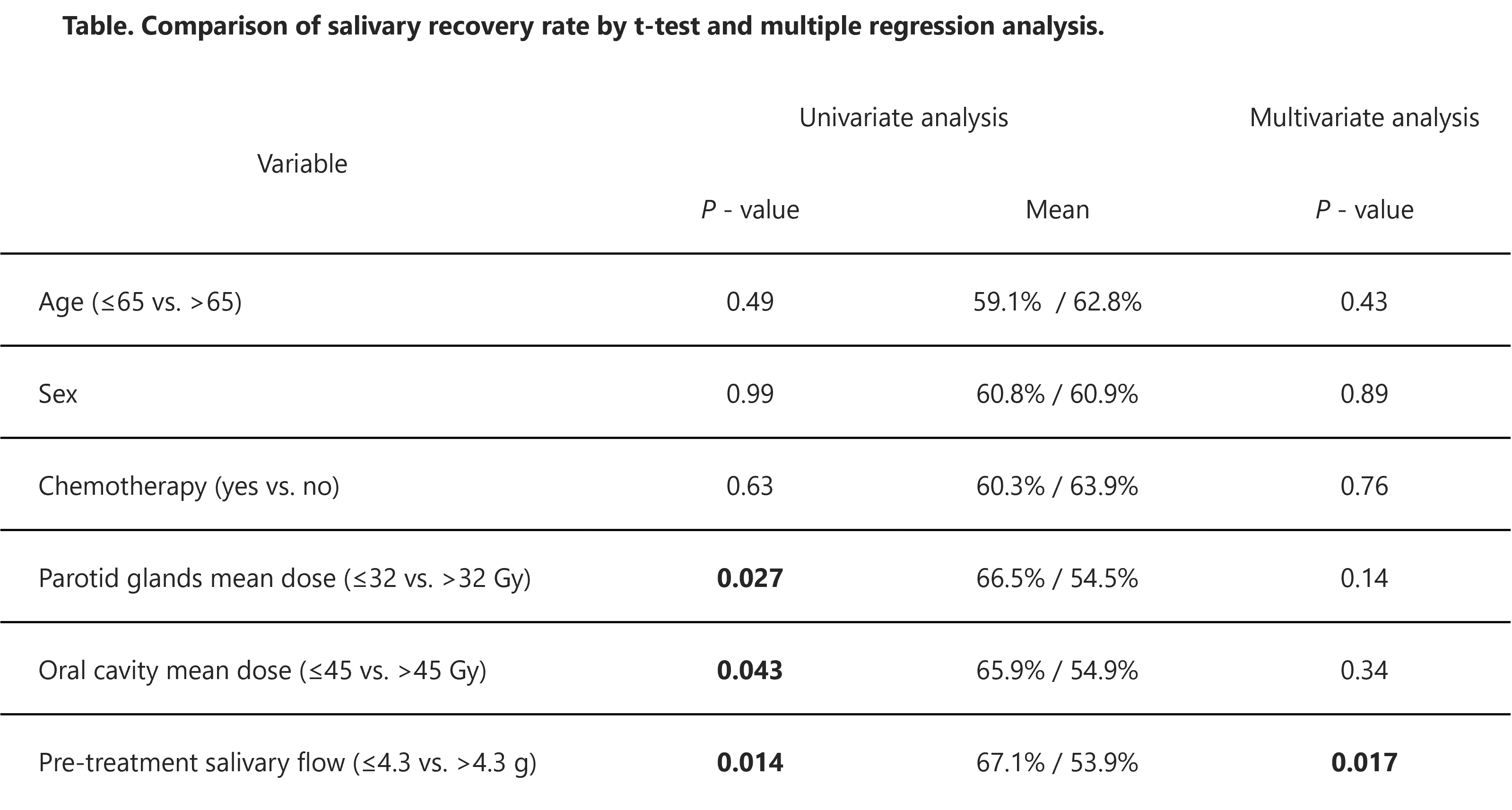
recovery time [Figure]. In the univariate analysis, the salivary recovery rate was
significantly lower in patients with higher mean parotid glands dose, higher mean
oral dose, and higher pre-treatment salivary flow. In multivariate analysis,
only pre-treatment salivary flow remained a significant factor [Table]. Patients
with a higher grade of xerostomia had a lower salivary recovery rate (P <
0.001).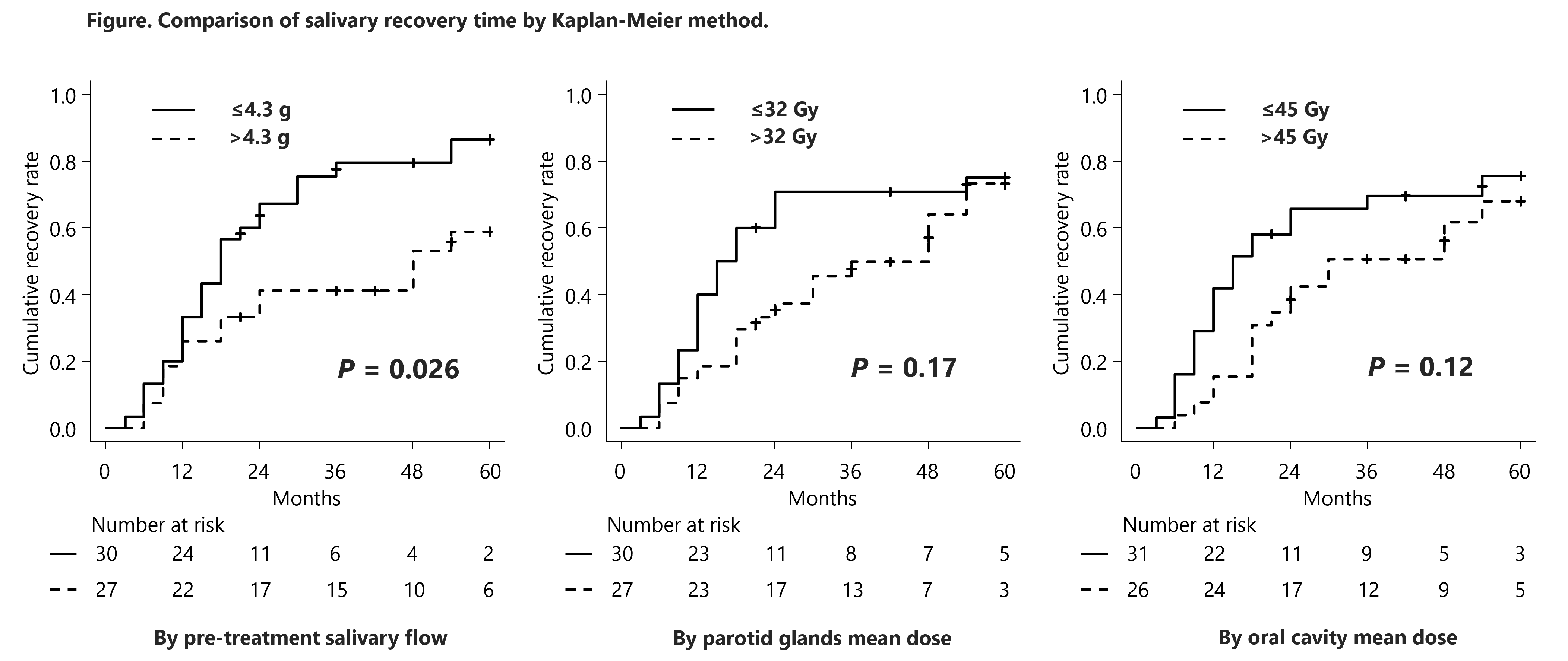
Conclusion
Patients with higher pre-treatment salivary flow
experienced slower and lower salivary recovery rates. Parotid glands and oral
cavity mean doses were not significantly associated with salivary recovery time.
Parotid glands and oral cavity doses should be reduced as much as possible, even
for patients with high pre-treatment salivary flow.