GTV as prognostic marker in head and neck cancer - Time to redefine GTV beyond contouring
PO-1091
Abstract
GTV as prognostic marker in head and neck cancer - Time to redefine GTV beyond contouring
Authors: Imtiaz Ahmed1, Sapna Krishnamurthy1, Rohan Bhise2, Raghavendra Sagar1, Boopalan Balaji1, Arya Devi1, Vahitha Banu1
1KLES Dr Prabhakar Kore Hospital and MRC, Radiation Oncology, Belgaum, India; 2KLES Dr Prabhakar Kore Hospital and MRC, Medical Oncology, Belgaum, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Precision
radiotherapy is the essence of modern day treatment for head and neck cancers,
which utilizes accurate delineation of target volumes for accurate dose
delivery. Volumetric measurement of the tumour depicts the number of clonogenic
cells present and thus can predict the treatment outcomes. This volume defined
as GTV in the routine radiotherapy planning has been limited for mere contouring
purpose and its potential as prognostic factor is less explored.
Material and Methods
The data of 150
patients of head and neck cancer undergoing IMRT and weekly
cisplatin (40mg/m2) between April 2015 and December 2019 at
our Institution were retrospectively analyzed. GTVp (primary), GTVn (node) and
GTVcombo (primary + node) contoured on eclipse treatment planning system
version 13 were used to generate the volumetric parameters. The prognostic
value of these tumour volumes with respect to treatment outcomes was analyzed
using SPSS version 16.
Results
Median age at presentation was 58.5 years. 73% were male. 42.6%,
36.6% and 20.6% had Oropharynx, Hypopharynx and Larynx primaries respectively. 16%,
62%, 19% and 3% had T2, T3, T4a and T4b disease; 32%, 23%, 41% and 3% had N0,
N1, N2 and N3 disease respectively. 50%
had stage III disease. Mean GTVp was 44.5cc (range 2.4 – 169.3), mean GTVn was
13.4cc (range 0 – 156.1) and mean GTVcombo was 57.9cc (range 2.4 – 227.2). All
patients completed 70Gy in 33-35 fractions; median chemotherapy cycles were 6.
64% had complete response (CR). Comparison of GTV with CR rates was done using
Pearson Chi-Square test, GTVp <30cc had better CR rates than GTVp >30cc (82.6%
v/s 51.9%, p=0.00), GTVn <4cc had better CR rates than GTVn >4cc (74% v/s
58.4%, p=0.04) and GTVcombo <50cc had better CR rates than GTVcombo >50cc
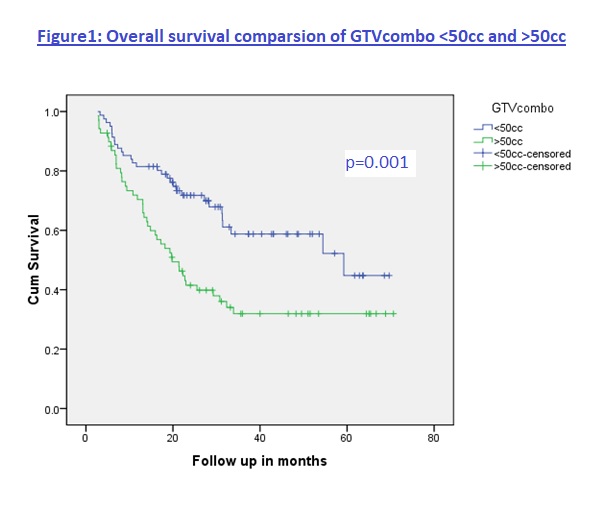
(81.5% v/s 47.8%, p=0.00). At median follow up of 21.4 months (range 3 – 71) OS
was 60% and median OS was 32.3 months. Estimated 3 and 5 year OS was 49% and
42%. On Univariate analysis the median OS
in patients with GTVp < 30cc was better than GTVp >30cc (59.2 v/s 21.4
months, p=0.003); GTVn <4cc was better than >4cc (59.2 v/s 22.2 months,
p=0.019); and GTVcombo <50cc was better than >50cc (59.2 vs 19.8 months, p=0.001).
Conclusion
GTV
should not just be limited for contouring but also has to be recognized as an important
prognostic factor.