Head and neck cancer of unknown primary: recurrence pattern based on treatment volumes
Annamaria Guaineri ,
Italy
PO-1086
Abstract
Head and neck cancer of unknown primary: recurrence pattern based on treatment volumes
Authors: Annamaria Guaineri1, Marta Maddalo2, Michela Buglione di Monale e Bastia2, Stefano Maria Magrini2, Cristian Toraci2, Paolo Bossi3, Alberto Paderno4, Roberto Maroldi5, Marco Ravanelli5, Cesare Piazza4, Salvatore La Mattina6, Giorgio Facheris2, Giulia Volpi2, Navedeep Singh2, Edoardo Pastorello2
1Ospedale Esine, Radioterapia, Esine, Italy; 2Spedali Civili, Istituto del Radio, Brescia, Italy; 3Spedali Civili , Oncologia, Brescia, Italy; 4Spedali Civili, Otorinolaringoiatria, Brescia, Italy; 5Spedali Civili, Radiodiagnostica, Brescia, Italy; 6Spedali Civili , Istituto del Radio, Brescia, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Optimal
management of head and neck cancer of unknown primary (HNCUP) is still
controversial. Radiotherapy (RT) is a main stem of HNCUP treatment. Also the choice of treatment volumes is controversial, in particular whether RT should be extended from the unilateral (UN) to the bilateral neck
(BN) and whether or not include the pharyngeal mucosa (PM). A detailed
understanding of treatment failure patterns is therefore essential.
Material and Methods
This is a
retrospective series of HNCUP patients (pts) treated between 2005 and 2020.
Pts, tumor and treatment characteristics have been correlated to survival
outcomes: overall (OS), progression free (PFS), local progression free (LPFS),
regional recurrence free (RRFS) and metastases free (MFS) survival. LPFS has
been defined as the time elapsed between end of treatment and appearance of the
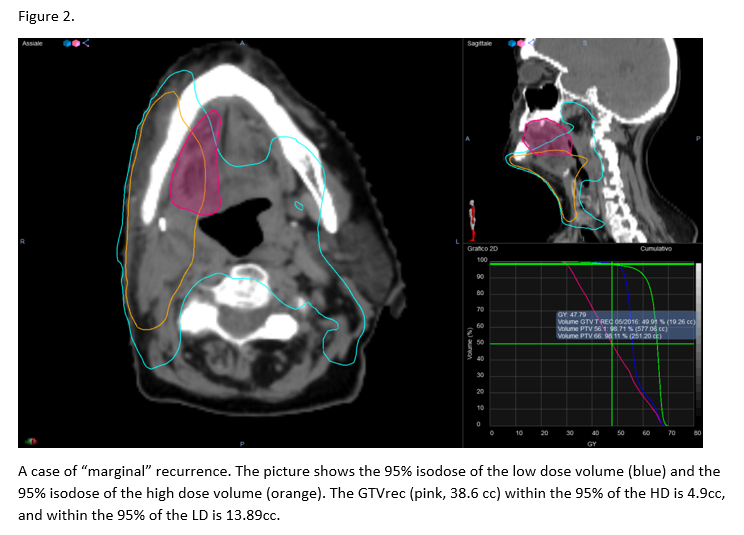
primary site of disease. MRI images of local/regional recurrences have been
co-registered with RT images and plan and the area of recurrenc e(GTVrec) has
been defined according to the prescribed dose received as “in-field” (>
80% of volume included in the 95% isodose), “out-of-field” (< 20% of
volume included in the 95% isodose) or “marginal”(intermediate situation).
Results
Of the 52
pts with HNCUP 7 (13.7%) had a local +/- regional recurrence. Nodal
presentation was unilateral in 67.3% of pts and the majority of pts (78.8%)
underwent a nodal dissection and adjuvant RT. RT volume was UN and BN in 28.8%
and 71.2% respectively; in 64.4% of pts RT volumes included also the PM. Mean dose to the high dose volume was 64.8 Gy, while mean dose to the low dose volume was 53.2 Gy. Concomitant
chemotherapy was used in 53.8% of cases. None of the variables analysed
correlated with OS. Presence of extranodal extension was the only variable
associated with PFS [p<0.000 HR 23.2 (CI 4.9-108.8)] and MFS [p<0.004 HR
11.98 (CI 2.2-65.93)]. LPFS was correlated with a synchronous nodal progression
[p<0.001 HR 13.01 (CI 2.9-59.3)] as no event of RRFS was seen in patients
with no appearance of the primary site. The primary site was oropharynx, oral
cavity and skin in 2, 4 and 1 pts respectively. Three pts had also a nodal
recurrence. After image co-registration 40% of relapses were in-field, 10%
marginal and 50% out-of-field. No differences were found in terms of RT volumes
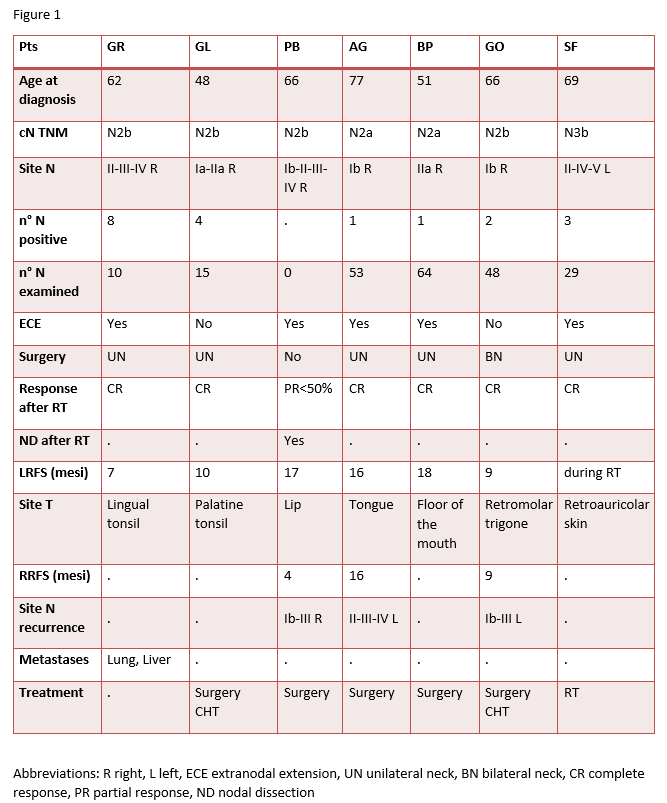
(UN versus BN, PM yes versus no) and evidence of relapse. Figure 1 summarizes
the characteristics of patients with local/regional recurrence. Figure 2 shows
an example of image co-registration.
Conclusion
Adequate
staging procedures can lead to the identification of the primary site in most
cases. Our data confirms thats in cases
of real HNCUP an intensified multimodal treatment and an extensive
nodal/mucosal coverage with RT have shown no benefit on survival outcomes. ENE
is closely linked to worse PFS and MFS and should prompt the investigation of
new therapeutic approaches. Due to the lack of clinical prognostic factors we support molecular and radiomic research in
better stratification of HNCUP.