Impact of multidisciplinary target review in head and neck radiation
PO-1085
Abstract
Impact of multidisciplinary target review in head and neck radiation
Authors: Kaoutar SOUSSY1, Sara RIDAI1, Akos GULYBAN2, Sofian BENKHALED3, Sylvie BEAUVOIS1, Yolene LEFEBVRE4, Elcin OZALP5, Marc LEMORT4, Manuela BURGHELEA6, Clémence AL WARDI7, Dirk VAN GESTEL1, Tatiana DRAGAN1
1Jules Bordet Institute, Radiotherapy, Brussels, Belgium; 2Jules Bordet Institute, Medical Physics, Brussels, Belgium; 3Jules Bordet Institut, Radiotherapy, Brussels, Belgium; 4Jules Bordet Institute, Radiology, Brussels, Belgium; 5Jules Bordet Institute, Nuclear medicine, Brussels, Belgium; 6Jules Bordet Institutes, Medical physics, Brussels, Belgium; 7Jules Bordet Institute, Radiotherapy (Research Coordinator), Brussels, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Target volume delineation remains the most critical part of the radiotherapy process especially for Head and Neck cancer (HNC) patients. In this study we aim to assess the added value of a weekly, joint multidisciplinary (dedicated radiation oncologists (RO), radiologists (RX) and nuclear medicine (NM) physicians) target definition team meeting (MTM) on the final primary and metastatic lymph node gross tumor volume (GTVp and GTVn) delineation.
Material and Methods
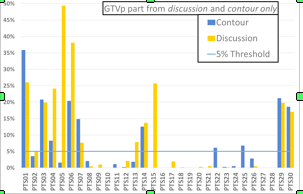
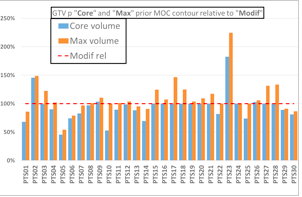
30 consecutive HNC patients referred for definitive curative radiotherapy were included in this study. All patients underwent head and neck MRI, PET and contrast enhanced CT scan prior radiotherapy. All cases with all imaging modalities were distributed to the multidisciplinary team. RX and NM were asked to delineate the primary GTV (GTVp_RX, GTVp_NM), while the RO first defined ‘undeniable’ tumor (GTVp_core), then enlarged towards a GTVp_max in case of doubt on the tumor extent. During the MTM these 4 contours were discussed and a GTVp_final was defined. For GTVn, interactive discussion was conducted and documented on the extent and malignancy of lymph nodes. For comparison of different GTVp, beyond the descriptive statistics, two evaluations were used: 1) added value of MTM delineation only, defined as part of GTVp_final outside the GTVp_core, but included in GTVp_RX and/or GTVp_NM and 2) the discussion defined as part of GTVp_final that was not part of the GTVp_max. For the GTVn discussion, clinical description of the source of disagreement was noted with its frequency.
Results
The GTVp core and max volumes were on average 17.5cc (r: 0.4-48.1) and 19.8cc (r: 0.8-58.7), respectively. GTVp_max was larger than core by a mean of 18% (r: 1-89%). The delineation contributed on average 1.7cc (range: 0-23.9) to the GTVp_final, while a mean of 2.3 cc (r: 0-21.3) was not included in the volume prior MTM. A mean of 8.7% (r: 0-49.4) and 6% (r: 0-35.9) would have been missed without delineation and discussion, respectively. Regarding GTVn the most frequent discussion included morphologically suspicious nodes, i.e. nodal size and contrast enhancement pattern on CT and/or MRI, not fixing on PET, followed by small PET negative retropharyngeal lymph nodes.
Conclusion
Delineation prior MTM and discussion during MTM can lead to substantial change in GTVp and GTVn. Further observation is planned to identify patters of disagreement, which will increase precision and reinforce the added value of the MTM.