Evaluation of Vascular and Nerve Changes in Nasopharyngeal Carcinoma Patients Following Radiotherapy
PO-1077
Abstract
Evaluation of Vascular and Nerve Changes in Nasopharyngeal Carcinoma Patients Following Radiotherapy
Authors: Meltem Dağdelen1, Zeynep Şerikoğlu Akbaş2, Ceren Barlas1, Günay Can3, Ceyhun Arıcı2, Ömer Uzel1
1Istanbul University- Cerrahpasa, Cerrahpasa Medical Faculty, Department of Radiation Oncology, Istanbul, Turkey; 2Istanbul University- Cerrahpasa, Cerrahpasa Medical Faculty, Department of Ophthalmology, Istanbul, Turkey; 3Istanbul University- Cerrahpasa, Cerrahpasa Medical Faculty, Department of Public Health, Istanbul, Turkey
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiation-induced optic neuropathy (RION) is
one of the most important late complications during head and neck
radiotherapy and is recognized usually between 2-9 years after RT. Our study aims to
prospectively evaluate retinal and optic disc vascular changes and retinal
nerve fiber layer thickness (RNFL) using optical coherence tomography
angiography (OCTA) in nasopharyngeal cancer (NPC) patients previously treated
with intensity-modulated radiation therapy (IMRT) and with optic nerve doses
are above 45 Gy
Material and Methods
Fourteen NPC patients and sixteen age-matched healthy
control subjects were included in our study. A complete ophthalmological examination
including the best-corrected visual acuity (BCVA), intraocular pressure,
slit-lamp biomicroscopic, fundoscopic examination, and OCTA were performed for
all patients and healthy volunteers. OCTA findings of RT and control groups
were compared and correlation analysis was performed to find the association
between the radiation-related factors and OCTA findings.
Results
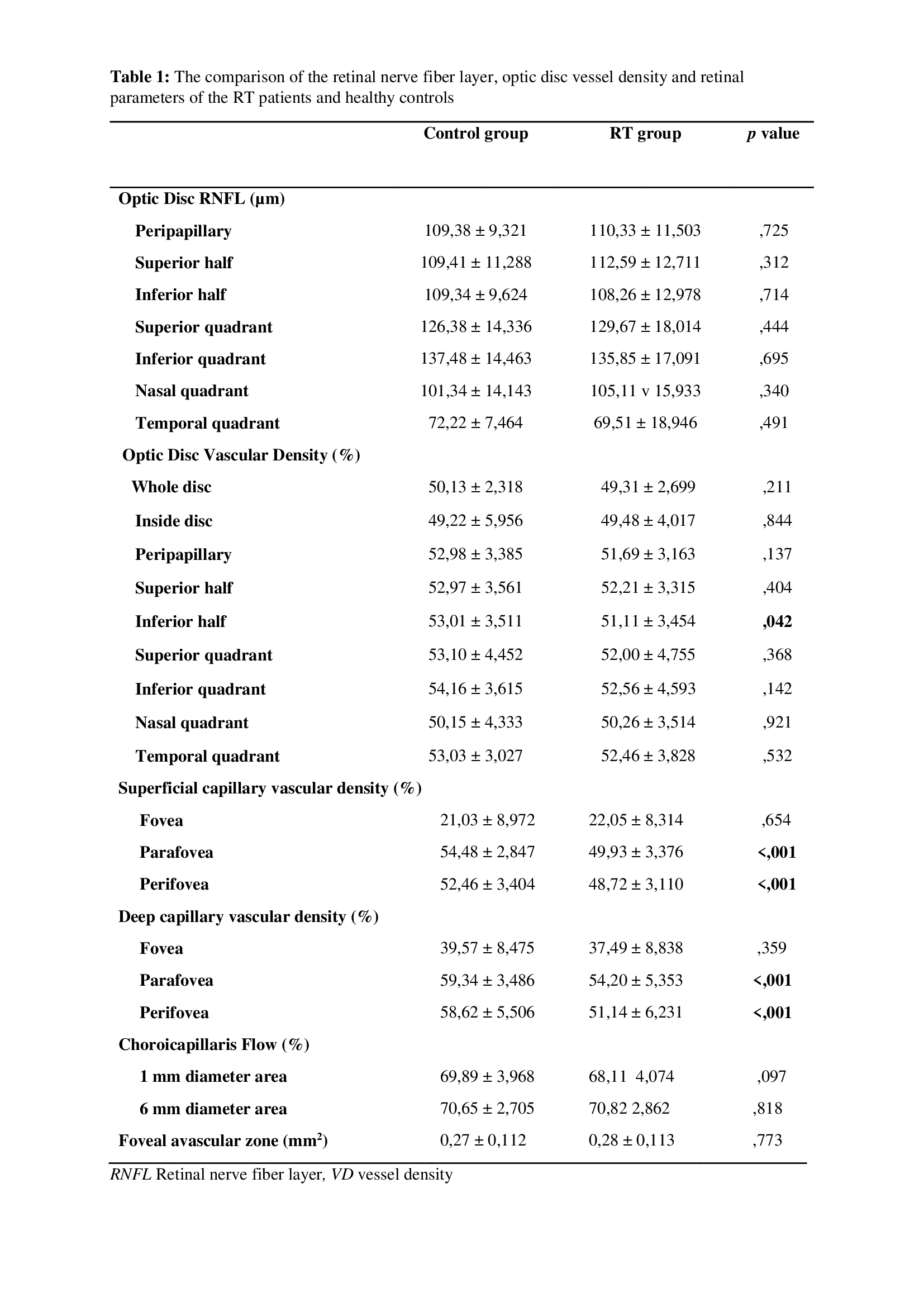
Inferior hemi disc, parafovea, and perifovea
superficial/deep vessel densities were statistically significantly lower in RT
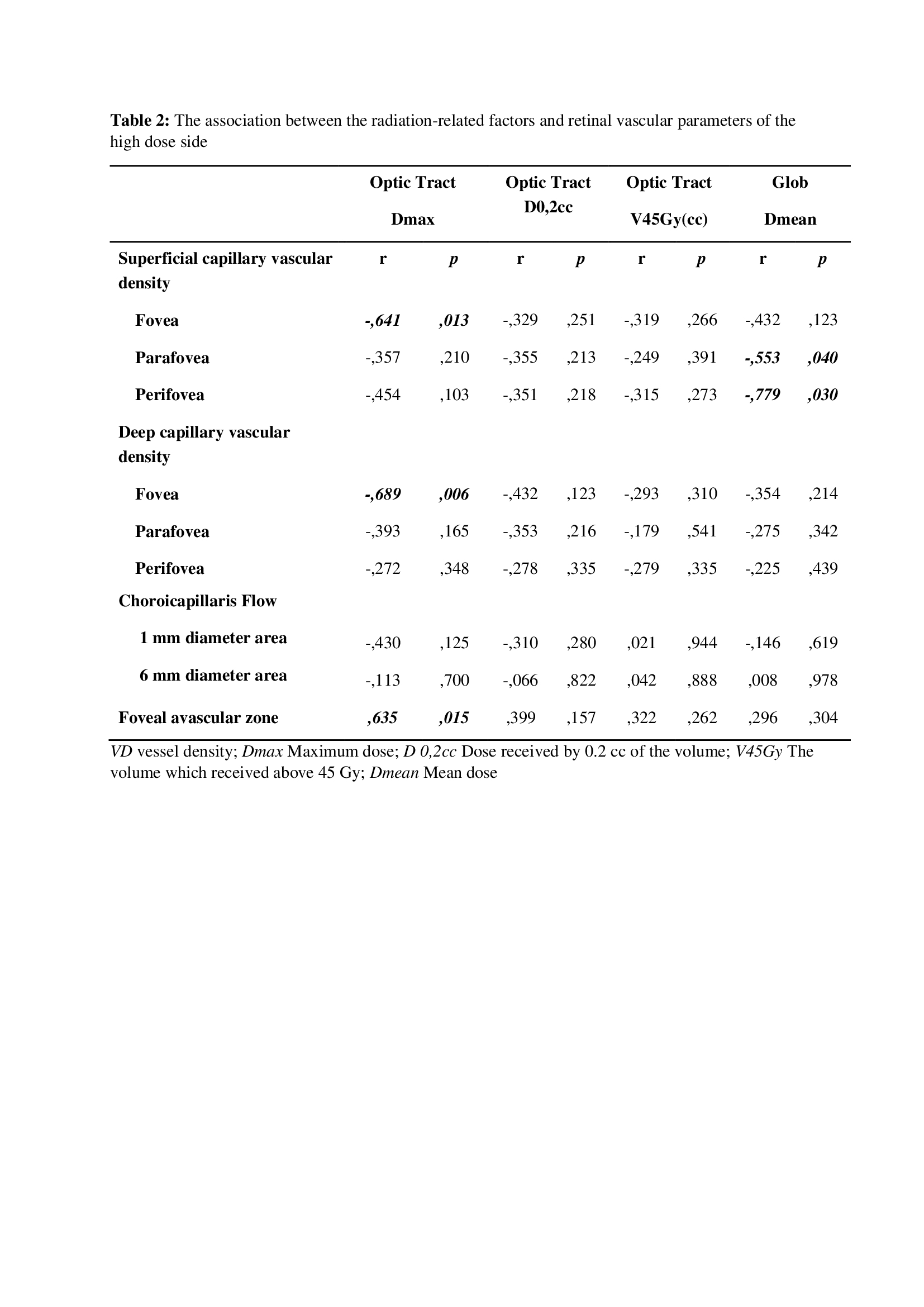
patients (Table1). Negative correlations were
found between Dmax of the optic tract and both RNFL and vessel densities.
Furthermore, there were negative correlations found between the Dmean of globe
and vessel densities(Table2).
Conclusion
Although none of the patients in our study had
marked vision loss and retinal abnormalities with the examination, OCTA
findings showed that perifoveal and parafoveal vascularity were
statistically significantly affected due to the RT.