Assessment of Catheter Displacement on Single Fraction HDR Prostate Brachytherapy Treatment
Andrew Nisbet,
United Kingdom
PD-0569
Abstract
Assessment of Catheter Displacement on Single Fraction HDR Prostate Brachytherapy Treatment
Authors: Siti Khairina Abdul Wahab1, Maria Boutros2, Gordon Sands2, Andrew Nisbet1
1University College London, Department of Medical Physics and Biomedical Engineering, London, United Kingdom; 2University College London Hospital, Radiotherapy Department, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
In CT-planned HDR prostate brachytherapy the time delay of ~2 to 3 hours between the insertion of catheters and treatment delivery may
bring about inaccuracies to the treatment delivery due to catheter
displacement. The catheter position in the scanned image, used to plan a
treatment, may not match the true positions in the patient during treatment. In
such cases, the catheters may need to be repositioned and the procedure
repeated. This prolongs the treatment procedure and may lower the quality of
the treatment. This study involves evaluating the impact of the catheter
displacement in single fraction HDR prostate brachytherapy treatment.
Material and Methods
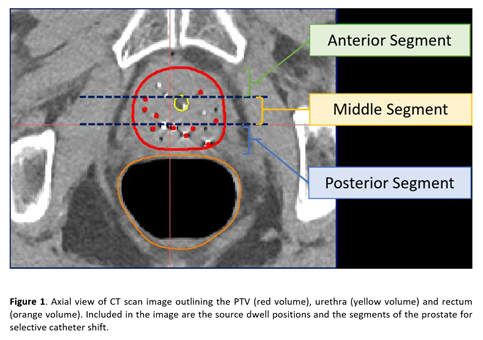
20
patients had simulated catheter displacement introduced on Oncentra Brachy. The
catheter shifts were simulated in two ways, synchronous and selective catheter
shift. For the former, for each treatment plan, all catheters were displaced
uniformly through known values. For the latter, catheters were selectively
displaced, based on the segment of the planning target volume (PTV) where they
were positioned; anterior, middle and posterior segment as shown in Figure 1.
The dose coverage to the PTV, urethra, bladder and rectum were then evaluated
using the parameters of dose coverage to 90% of the PTV volume, D90, dose
accumulated by 30% of the urethra volume, D30, and the volume of the bladder
and rectum receiving 70% (10.5 𝐺𝑦) of prescribed dose, V70.
Results
The
treatment planning goal for D90 is to deliver a minimum of 90% of the
prescribed dose. Majority of treatment plans for synchronous catheter shift
simulations show PTV dose coverage meeting this clinical constraint in the
range of −3𝑚𝑚 to 6𝑚𝑚. Increase in D30 of the urethra is seen as the catheters are
shifted inferiorly; bladder V70 increases as the catheters shift superiorly;
and as the catheters shift inferiorly, more of the rectal V70 accumulates. For
selective catheter shift simulation, a significant dose increase to the PTV was
detected at 3𝑚𝑚 superiorly upon shifting
the catheters in the middle segment for all patient groups. For urethral D30, a
distinct dose increase is observed in the results for the ‘anterior segment’
and ‘posterior segment’ catheter shift as the shifts increase inferiorly.
However, simulating the inferior shifts for the ‘middle segment’ catheters
resulted in a random dose fall-off to the urethra. There is an increase in V70
for the bladder as the catheters shift superiorly, and for the rectum, dose
increase is observed when catheters in the posterior segment shift inferiorly.
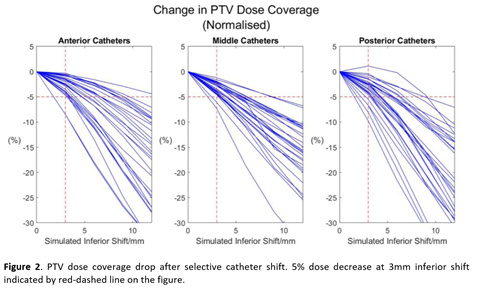
To estimate the needle shift tolerance, the normalised dose coverage drop to
the PTV is plotted using the data from the selective catheter shift simulation,
see Figure 2.
Conclusion
Approximately 90% of all treatment plans
experience a dose decrease of less than and equal to 5% when the catheters were
displaced by 3𝑚𝑚. To ensure PTV dose coverage is maintained at an optimum level and to
reduce organ toxicity, the needle shift tolerance has been concluded to be 3𝑚𝑚.