Anatomy- versus margin-based prophylactic para-aortic radiotherapy in cervical cancer
Jie Lee,
Taiwan, Province of China
PD-0908
Abstract
Anatomy- versus margin-based prophylactic para-aortic radiotherapy in cervical cancer
Authors: Jie Lee1, Jhen-Bin Lin2, Chih-Long Chang3, Yu-Jen Chen1, Meng-Hao Wu1
1MacKay Memorial Hospital, Radiation Oncology, Taipei, Taiwan; 2Changhua Christian Hospital, Radiation Oncology, Changhua, Taiwan; 3MacKay Memorial Hospital, Obstetrics and Gynecology, Taipei, Taiwan
Show Affiliations
Hide Affiliations
Purpose or Objective
Prophylactic para-aortic radiotherapy (PART) can
mitigate the risk of para-aortic recurrence in locally advanced cervical cancer
(LACC). However, target volume delineation for the para-aortic region is inconclusive. Based on studies evaluating the mapping of para-aortic nodes,
margin expansions around the aorta and inferior vena cava (IVC) were suggested
to achieve coverage of para-aortic region. However, anatomic principles that
govern the distribution of lymphatics may more accurately define the
para-aortic regions that determine the effectiveness and potentially reduce the
dose to the intestine and further lower incidence of gastrointestinal (GI) toxicity.
This study aimed to compare patient-reported GI toxicity and outcomes between
anatomy- and margin-based prophylactic PART in patients with LACC.
Material and Methods
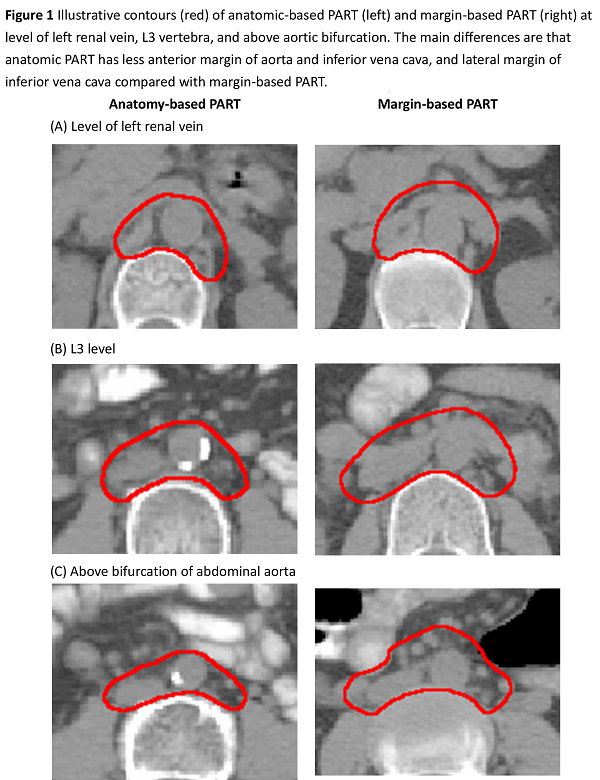
We reviewed data of 160 patients with LACC who underwent CCRT with prophylactic PART
during 2014–2019 at two tertiary medical centers. Para-aortic regions were
drawn by margin expansion of 7–10 mm around aorta and IVC or anatomic
para-aortic region atlas published by Takiar et al. (Figure 1). The upper border
of PART was at the level of left renal vein. The prescribed dose of PART was 45
Gy. Patient-Reported Outcome version of the Common Terminology Criteria for
Adverse Events (PRO-CTCAE) was used to assess acute GI toxicity. Vx indicated
the volume (mL) of small bowel or duodenum that received a radiation dose of x
Gy.
Results
Eighty-four and 76 patients received
margin-based and anatomy-based PART, respectively. Median follow-up time was 40.1
months (IQR: 25.5–58.9). The V45 and V30 of small bowel and duodenum were
significantly lower in the anatomy-based PART group compared with margin-based
PART group (small bowel, V45: 159.6 ±
32.8 vs. 188.7 ± 47.4, p<0.001;
V30: 615.3 ± 131.0 vs. 742.6 ± 127.1, p<0.001;
duodenum, V45: 8.3 ± 3.9 vs. 16.1 ± 5.9, p<0.001;
V30: 19.8 ± 6.2 vs. 26.9 ± 6.4, p<0.001,
respectively). The V15 of small bowel and duodenum were not significantly
different between groups. Patients who received anatomy-based PART
experienced significantly less patient-reported severe toxicity (PRO-CTCAE
score ≥3) than patients who received margin-based PART in terms of frequency of
diarrhea (7.9% vs. 20.2%; p=0.03),
severity of abdominal pain (3.9% vs. 14.3%; p=0.03),
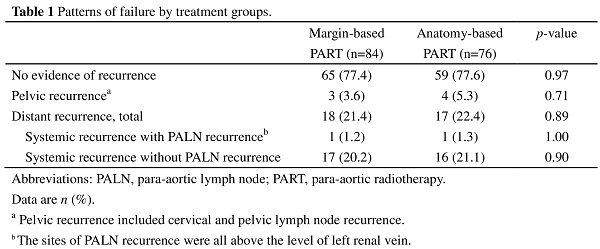
and interference of abdominal pain (2.6% vs. 11.9%; p=0.03). The patterns of failures were not different between groups
(Table 1). The sites of PALN
failures of these two patients were above the level of left renal vein. There
was no in-field or marginal PALN failure in these two groups. The 3-year overall
survival and disease-free survival for margin-based PART vs. anatomy-based PART
were 80.9% vs. 84.9% (p=0.61) and 71.8%
vs. 77.4% (p=0.47), respectively.
Conclusion
Anatomy-based PART can reduce the dose-volume to
the small bowel and duodenum, and lower the incidence of severe
patient-reported GI toxicity. The patterns of failure and survival outcomes
were similar between para-aortic delineations.