Systemic treatment and ablative therapies in oligometastatic breast cancer: a single center analysis
Gauthier Glemarec,
France
PD-0749
Abstract
Systemic treatment and ablative therapies in oligometastatic breast cancer: a single center analysis
Authors: Gauthier Glemarec1, Jean Louis Lacaze2, Bastien Cabarrou3, Richard Aziza4, Eva Jouve5, Slimane Zerdoud4, Eleonora De Maio2, Carole Massabeau1, Maxime Loo1, Vincent Esteyrie1, Mony Ung2, Florence Dalenc2, Françoise Izar1, Ciprian Chira1
1Institut Claudius Regaud, IUCT-O, Department of Radiation Oncology, Toulouse, France; 2Institut Claudius Regaud, IUCT-O, Department of Medical Oncology, Toulouse, France; 3Institut Claudius Regaud, IUCT-O, Biostatistics Unit, Toulouse, France; 4Institut Claudius Regaud, IUCT-O, Department of Radiology, Toulouse, France; 5Institut Claudius Regaud, IUCT-O, Department of Surgery, Toulouse, France
Show Affiliations
Hide Affiliations
Purpose or Objective
Although
metastasis-directed therapy (MDT) with curative intent is increasingly added to
systemic treatments in oligometastatic breast cancer (OMBC), high-level
evidence to support this strategy is lacking. We aimed to evaluate the
addition of MDT to systemic treatment alone (STA) in terms of progression-free survival
(PFS) and overall survival (OS). Secondary endpoints were local control (LC) and
toxicity. We also sought to identify prognostic factors associated with
improved OS and PFS.
Material and Methods
OMBC patients were
screened from our institutional tumor board registry between 2014 and 2018.
OMBC patients with ≤ 5 metastatic de novo or recurrent lesions without central nervous
system involvement were included. We excluded patients with oligoprogressive
disease or uncontrolled loco-regional recurrence. MDT included stereotactic body radiation therapy (SBRT), surgery, percutaneous
radiofrequency ablative (PRA) and cryotherapy. Various radiation dose-fractionation schedules were used:
27Gy in 3 fractions for bone lesions, 50Gy in 5 fractions for lung tumors and
50-63.8Gy in 25-29 fractions for lymph node metastases. A Cox model
with time-dependent variable was used to study the impact of MDT on PFS and OS. Sensitivity
landmark analyses were also performed at 3 and 6 months.
Results
One hundred sixty OMBC
patients were identified and 102 were included (STA, n=62, MDT, n=40). Fifty two percent were
synchronous oligometastatic and 48% were oligorecurrent. Most patients had only
one metastasis (n=54, 52.9%). Most metastases were located in bone structures
(n=100, 53.2%), lymph nodes (n=37,19.7%) and liver (n=35,18.2%). Patients had one (n=88, 86.3%) or two metastatic sites
involved (n=14, 13.7%). Seventy two percent of patients had an FDG-PET/CT
examination of metastatic spread. Median follow-up was 50.4 months (95% CI
[44.4 ;53.4]). Five-year PFS and OS were 34.75% (95% CI
[24.42;45.26]) and 63.21% (95% CI [50.69; 73.37]) respectively.
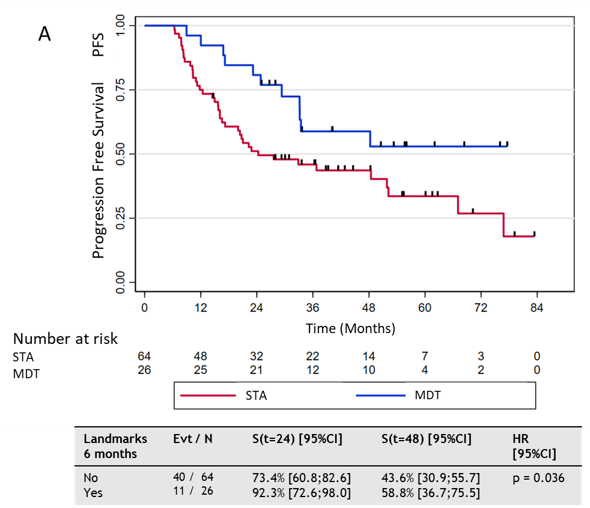
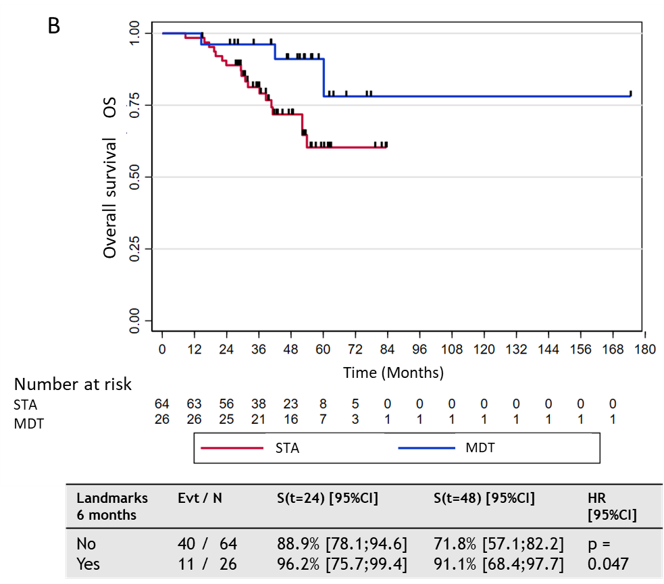
Patients receiving MDT and systemic treatment had a statistically significant
improved PFS and OS than those with STA ([HR 0.39, p=0.002]) and ([HR 0.31,
p=0.01]). Six months Landmark analyses after the
start of the first treatment showed a significant increase in PFS and OS between
patients with MDT and those with STA (Figure A and B). MDT was well
tolerated, only one patient presented grade 3 toxicity (pneumothorax) after
PRA. Bone metastases were associated with favorable PFS and OS in univariable analysis but
did not reach significance in multivariable analysis. In multivariable
analysis, MDT, HER2-positive status and hormone-receptor positivity were
associated with improved PFS and OS. Liver metastases led to worse PFS.
Conclusion
MDT seems to improve
outcomes in synchronous or recurrent OMBC when added to STA without a
significant increase in toxicity. The prognostic factors of PFS and OS that we
identified may guide clinicians in selecting patients for MDT but need
confirmation from other studies.