Eighty
patients with 114 lesions were included, of these, 59 (52%) were treated with
CPAP-FB and 55 (48%) were treated with CPAP-DIBH. Median radiation dose was
51.8 Gy, median biological effective dose (BED10) was 111Gy. The
groups were balanced with respect to age, gross tumor volume (GTV), radiation
dose, tumor location and prior lung radiation. Lung volume in CPAP-DIBH group
was 5273ml (SD1178), significantly larger than CPAP-FB:3932ml (SD1082) (p=0.001) CPAP-DIBH had smaller
planning target volume (PTV) 21 cm3 (SD30) vs. 33 cm3 (SD33)
in CPAP-FB (p=0.02). With median FU of 21.7months, the LC at 2 years for the
entire cohort was 73.5% (95% CI 62-82%); for stage-1 lung cancer 2-yrs LC was 88% (95% CI 59-97%) and for
metastatic cancer 70% (95% CI 57-80%). On univariate
analysis, LC was improved with GTV≤3cm3 (HR 4.6, p=0.001), use of
CPAP-DIBH (HR 2.5, p=0.04) and non-colon cancers (HR 2.8 p=0.014)(Figure 1A-D). Local
control was not affected by location at lower lobes (HR 0.8, p=0.5) and BED
(10) <105 Gray (HR 0.54, p=0.24). These associations remained
significant for LC using CPAP-DIBH (p<0.0001), GTV≤3cm3 (p=0.001) and non-colon cancer (p=0.0001) on multivariate analysis.
Tolerability was favorable: all patients who
started also completed treatment, except for one patient who suffered syncope
(m/p unrelated).
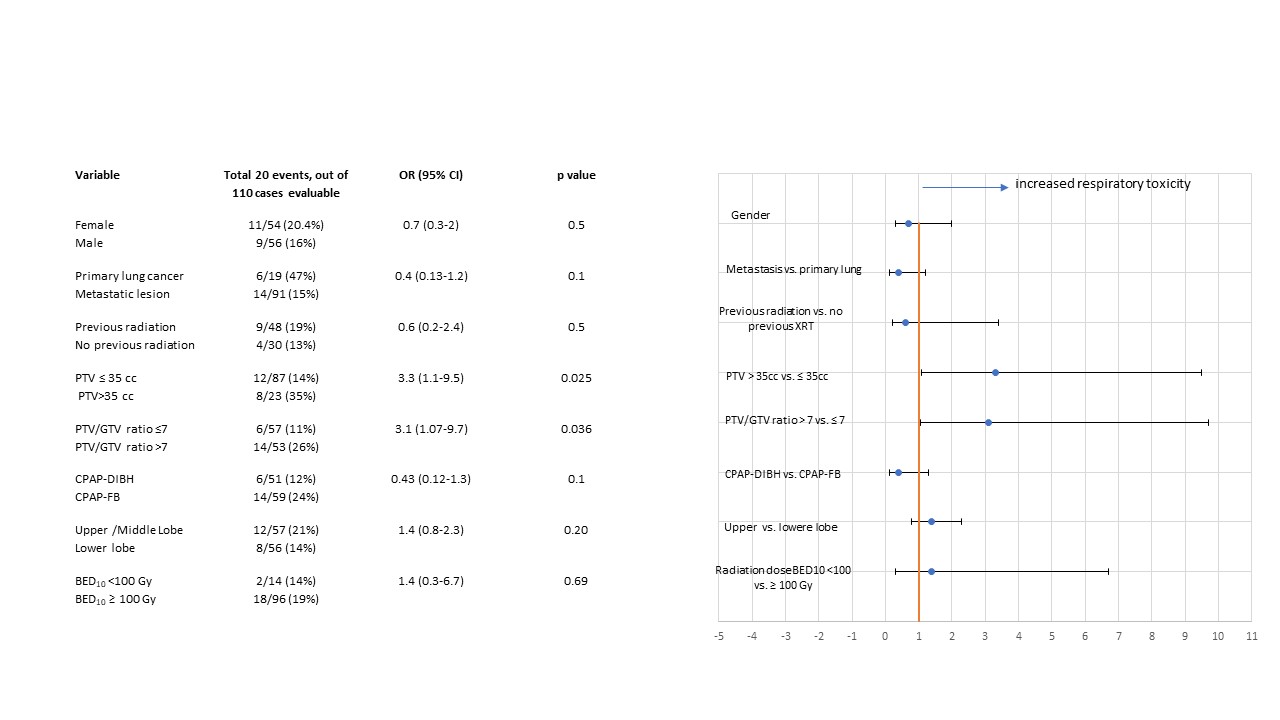
Respiratory toxicity grade 2-3 occurred in
20/110 cases, and was reduced with CPAP-DIBH 6/51 (12%) vs. CPAP-FB 14/59 (24%)
(OR 0.43, p=0.1). Respiratory toxicity correlated with larger PTV>35cm3
(OR 3.3, p=0.025) and PTV/GTV ration>7 (OR 3.1,P=0.036) (table 1).
At 6- and 12-months mass-like pattern
consolidation was recorded in 18.3% and 24%; modified conventional pattern consolidation
in 30.3% and 31%. Late consolidations correlated with larger PTV>35cm3
(OR 4.6, p=0.026), lower lobe location (OR 2.7, p=0.03), and trended to be reduce
with CPAP-FB compared with CPAP-DIBH (OR 0.6, p=0.3).
Figures 1A-D:
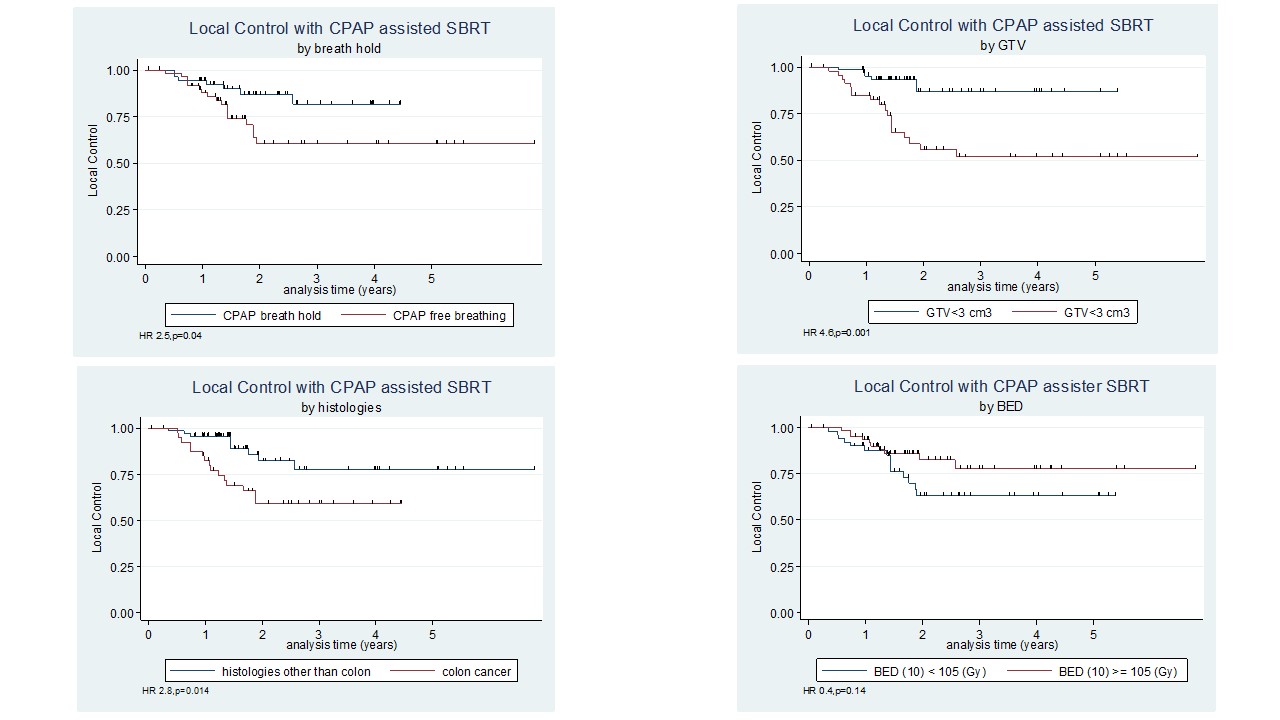
Table 1