There were 243
courses of RT and 50 courses (20.6%) of hypo-RT. Median age was 72.6 years at
diagnosis (range: 28.6-101.0) and median follow-up was 37.8 months (range:
1.2-194.5). Compared to the conv-RT group, the hypo-RT group had a similar proportion
of immunosuppressed pts (12.0% vs. 13.0%, p=1.00), and use of definitive RT (48.0%
vs. 33.2%, p=0.07), but was more likely to be ≥73 years at diagnosis (78.0% vs.
41.5%, p<0.01), receive an equivalent total dose in 2-Gy fractions (EQD2)
<50 Gy (58.0% vs. 5.2%, p<0.01), and undergo RT after 2016 (72.0% vs.
38.9%, p<0.01). While 3-year overall survival (OS; 53.4% vs. 77.4%,
p<0.01) was expectedly lower in the hypo-RT cohort, 3-year MCC-specific
survival (84.5% vs. 82.6%, p=0.76) was not different, and only 2 (4.0%) and 2
(1.0%) pts recurred within the irradiated region in the hypo-RT and conv-RT
groups, respectively. The most common sites of first recurrence were distant (14.0%
vs. 15.0%) and in-transit metastases (8.0% vs. 7.8%) in hypo-RT and conv-RT
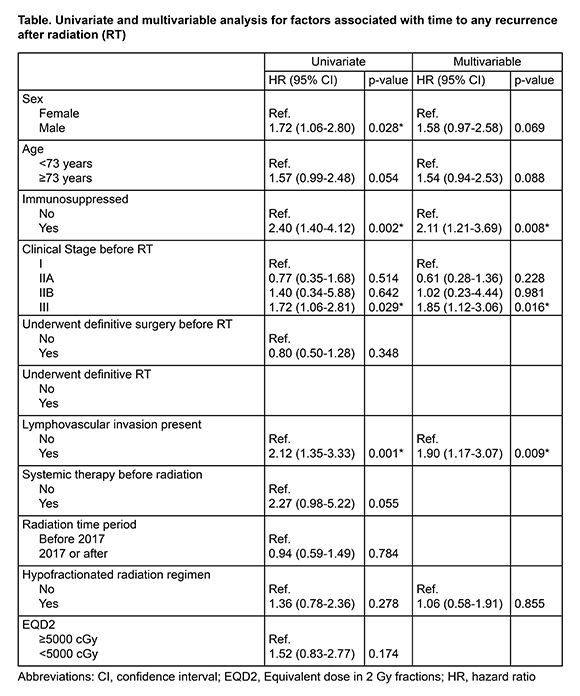
groups, respectively. On UVA, male, immunosuppression, clinical stage III, and lymphovascular
invasion (LVI) was associated with decreased time to any recurrence, but
hypo-RT was not (hazard ratio [HR] 1.36, 95% confidence interval [CI]: 0.78-2.36,
p=0.28), and definitive RT was not (HR: 1.23, 95% CI: 0.77-1.96, p=0.39). On MVA,
immunosuppression (HR: 2.11, 95% CI: 1.21-3.69, p=0.01), clinical stage III
disease (HR 1.85, 95% CI: 1.12-3.06, p=0.02), and LVI (HR 1.90, 95% CI: 1.17-3.07,
p=0.01) remained significant when controlling for sex, age, and hypo-RT (Table).