Reduced tube feeding dependence by continuous improvements in head and neck radiotherapy
Lisa Van den Bosch,
The Netherlands
OC-0088
Abstract
Reduced tube feeding dependence by continuous improvements in head and neck radiotherapy
Authors: Lisa Van den Bosch1, Hans Paul van der Laan1, Arjen van der Schaaf1, Johanna G.M. van den Hoek1, Edwin Oldehinkel1, Tineke W.H. Meijer1, Hans H.G. Verbeek1, Roel J.H.M. Steenbakkers1, Johannes A. Langendijk1
1University Medical Centre Groningen, Radiation Oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
The
aim of this study was 1) to assess the
prevalence of tube feeding dependence (TFD) during the course of radiotherapy in
head and neck cancer (HNC) patients treated over a time span of 13 years of
technological improvements and improved organ sparing capabilities and 2) to build
and validate NTCP models to estimate the benefit of proton therapy (IMPT) over
VMAT with regard to reducing TFD.
Material and Methods
The
study population was composed of 1181 HNC patients who underwent definitive
(chemo)radiation. Patients were treated with parotid sparing (ParRT:
2007-2010), swallowing sparing (SwRT: 2011-2017, including additional sparing
of pharyngeal constrictor muscle (PCM), supraglottic larynx and oesophageal inlet muscle) or multi-organ
sparing (MoRT: 2018-2020, including additional sparing of oral cavity and
submandibular glands) radiotherapy (Figure 1). All patients were subjected to a
prospective data registration protocol in which TFD (CTCAEv4.0 grade 4
dysphagia) was scored at baseline (BSL), weekly during treatment and at week 12. Dose-volume
data for a wide range of OAR were collected for the clinical plan and (in the
case of IMPT) the backup VMAT plans. First, the prevalence of TFD was studied
for the aforementioned three subsequent time periods. Subsequently,
multivariable NTCP modelling was performed in development (2007-2016) and
validation (2017-2020) cohorts using recently reported methods (R&O 148,
p.151; R&O 157, p.147). NTCP models were used for model-based clinical
validation and for estimating the clinical benefit of proton therapy in 135 patients
receiving IMPT.
Results
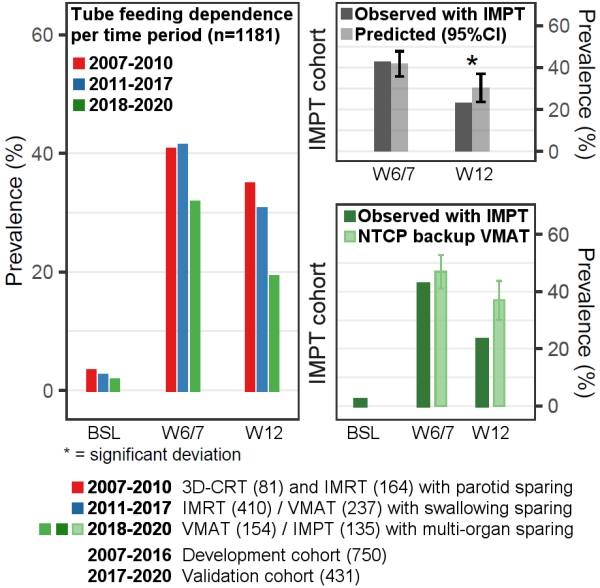
The
prevalence of TFD was 40.7%, 41.3% and 31.7% (last week of RT, W6/7) and 34.9%, 30.6%
and 19.2% (week 12) during ParRT, SwRT and MoRT, respectively (Figure 1). The predictors
for the final models were: Oral cavity Dmean; Superior PCM Dmean; Accelerated
radiotherapy; Chemoradiation; and Bioradiation. With MoRT, TFD in the last week
of RT was 31.7%, which was lower than predicted (34.5%, 95%CI: 30.6-38.3%). In
week 12, the prevalence of TFD was 19.2%, also lower than predicted (24.9%,
95%CI: 20.7-29.1%). The NTCP of TFD with the clinical Mo-IMPT plans was reduced
with 5.1 (46.9-41.8) and 6.6 (36.9-30.3) percent point in the last week of RT
and in week 12 as compared with the backup Mo-VMAT plans. The observed
prevalence with IMPT was 4.2 (46.9-42.7) and 13.7 (36.9-23.2) percent point
lower than the NTCP predicted for the backup Mo-VMAT plans in the same weeks,
respectively (Figure 1).
Conclusion
A marked
decline of TFD during treatment for head and neck cancer was observed during 13 years of continuous
technological improvements and improved organ sparing capabilities. In a recent
cohort of patients treated with multi-organ sparing VMAT or IMPT the prevalence
of TFD was even lower than expected. IMPT further reduces the NTCP of TFD with
5-7 percent point compared with VMAT, and with IMPT recovery of TFD seems even
better than expected in the weeks following RT.