Analysis Of A Mono-Institutional Internal Procedure Protocol During Covid-19 Second Wave
PO-1051
Abstract
Analysis Of A Mono-Institutional Internal Procedure Protocol During Covid-19 Second Wave
Authors: Marco Lucarelli1, Luciana Caravatta1, Antonietta Augurio1, Annamaria Vinciguerra1, Monica Di Tommaso1, Domenico Genovesi1,2
1SS. Annunziata Hospital, Department of Radiation Oncology, Chieti, Italy; 2G. D’Annunzio University, Department of Neuroscience, Imaging and Clinical Sciences, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Italy was one of the most affected
countries in Europe by COVID-19 pandemic. Starting from October 2020 to
February 2021, a new increment of contagion has been reported. It affected our
district more harshly than first wave: 92.5% of confirmed infections and 70% of
reported deaths happened in the examined four-month period. During the national lockdown, we ensured
Radiotherapy (RT) activities with a reorganization of our Unit according to a
specific internal procedure protocol, as reported in a previous publication. This
protocol was adopted in order to manage the emergency of the second wave. Specific
national and international guidelines were also adopted for a wider use of hypo-fractionated
RT.
Material and Methods
RT activity during the second wave was
analyzed according to a specific internal procedure protocol and Ministry of
Health recommendation concerning a reorganization of visits workloads and RT planning,
definition of dedicated routes and triage areas, management of suspected and
positive COVID-19 cases, use of personal protective equipment, management of
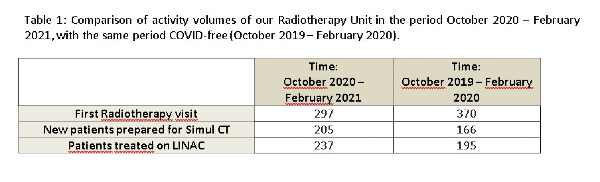
environments and management of intra-institutional meetings and tumor boards. A comparison of activity
volumes of RT Unit in the period (October 2020–February 2021) with the same but
COVID-free period of the last year (October 2019–February 2020) was made.
Results
In the checked four-month period, 297 first RT
visits were performed, 205 new patients were prepared for Simulation Computed
Tomography (Simul CT) and 237 patients were treated on one LINAC. In the same
period of 2019-2020, 370 patients underwent first RT visits, 166 new patients
were prepared for Simul CT and 195 patients were treated on one LINAC (Table 1). No positive cases of COVID-19
infection were recorded in healthcare professionals. There were 3 cases of
COVID-19 positivity among treated patients, with a median RT interruption of 11
days (range: 1-21). Finally, 3 new protocols for clinical trials using high conformal and short course RT
(accelerated partial breast RT, dose-intensification in short course RT for
rectal cancer and ultra-hypo-fractionated stereotactic RT for prostate cancer)
were proposed and approved by institutional tumor board and ethics committee.
They are currently on-going in clinical practice.
Conclusion
Although the number of first visits was slightly lower during the second
wave, the number of planned and treated patients did not decrease, according to
the workload of our radiation unit. These data confirmed the efficacy of our organizational
model planned to guarantee an optimal continuity of RT courses without workload
reduction nor treatments interruption and ensuring safety of cancer patients,
environments and radiation oncology staff, as reported in the previous
experience during the first wave of pandemic.