MRI-only from an economic perspective: Can new techniques in prostate radiotherapy be cost-saving?
PO-1044
Abstract
MRI-only from an economic perspective: Can new techniques in prostate radiotherapy be cost-saving?
Authors: Emilia Persson1,2, Niklas Svanberg1, Jonas Scherman1, Christian Jamtheim Gustafsson1,2, Adam Fridhammar3, Frida Hjalte3, Sven Bäck1, Per Nilsson1, Adalsteinn Gunnlaugsson1, Lars E. Olsson1,2
1Skåne University Hospital, Radiation Physics, Department of Hematology, Oncology, and Radiation Physics, Lund, Sweden; 2Lund University, Department of Translational Medicine, Medical Radiation Physics , Malmö, Sweden; 3The Swedish Institute for Health Economics, Health Economics, Lund, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
Cost and
time efficacy as well as reduced systematic uncertainties have been the main
motives for MRI-only radiotherapy (RT). Reduced registration uncertainty may be
exchanged to reduced treatment margins and smaller treatment volumes. However,
implementation of new techniques may increase complexity (e.g. additional QA),
which is associated with additional costs.
The aim of
this study was to analyze the actual costs of an MRI-only workflow in
comparison to a combined CT/MRI workflow for treating prostate cancer. Further,
the economic aspects of MRI-only prostate RT were assessed using late rectal
bleeding as a model for side effects.
Material and Methods
Following a
documented clinical implementation at Skåne University Hospital all tasks and
their associated costs were registered for MRI-only as well as for the CT/MRI workflow.
During an initial development phase, QA procedures specific for MRI-only were
assumed necessary, while these were excluded for long-term clinical use. The
synthetic CT (sCT) cost can vary widely between methods and was set as unknown
to generalize the calculation (=0). Price lists from 2019 were used for cost
estimations.
Treatment
plans for PTV margins of 5-10 mm were created and optimized for ten prostate
cancer patients prescribed 78Gy/39 fractions. The risk of grade 2+ late rectal
bleeding for each plan was calculated using the QUANTEC recommended NTCP model**.
The cost of late rectal bleeding was calculated by multiplying the estimated
risk of the side effect for the study population with the costs related to the
required diagnostic examinations (rectoscopy and hospital visits). Medical or
pharmaceutical treatment of the side effect and change in quality of life were
not considered.
Results
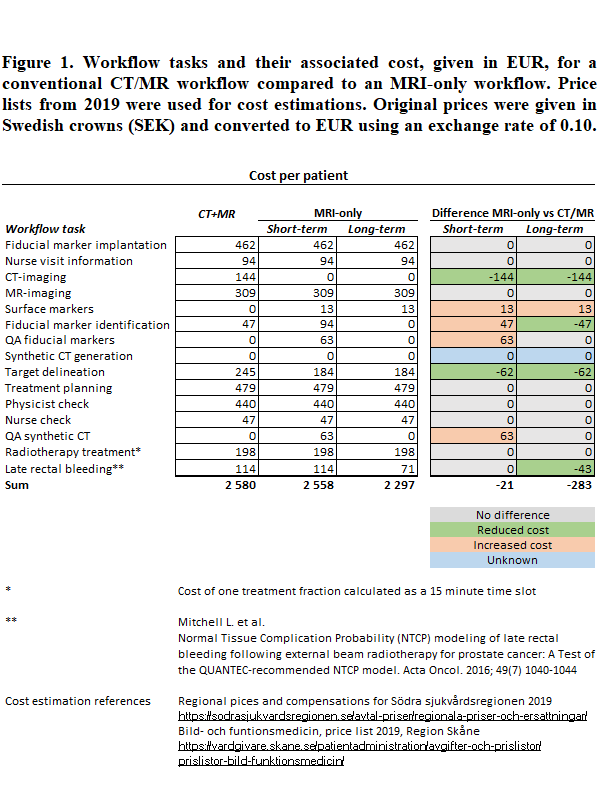
Associated
costs for the MRI-only implementation are shown in Figure 1. Excluded CT
examination and faster target delineation were the main contributors to cost
reductions. Additional QA procedures for fiducial marker identification and the
sCT limited the short-term cost reduction to 21 EUR/patient. On long-term use, assuming
a more time efficient workflow in combination with excluded extra QA, costs were
reduced by 240 EUR/patient.
A margin
reduction from 7 to 5 mm resulted in a mean population probability of late
rectal bleeding of 9.7% and 6.0%, respectively. With an associated diagnostic cost
of 1180 EUR/patient, the 2 mm margin reduction resulted in a reduced cost of 43
EUR/patient.
Conclusion
The
implementation of an MRI-only workflow is associated with reduced costs due to
time efficacy as well as reduced rectal toxicity, compared to a combined CT/MR
workflow. For MRI-only radiotherapy to be cost-saving, the sCT cost should not
exceed 283 EUR/patient.
The main
contributor of the MRI-only cost reduction is exclusion of the CT-examination.
On a short-term basis, the economic benefit is limited due to the extra costs
of QA procedures. The economic benefits of MRI-only are first seen when the
workflow is well established, and margin reduction has been included.