Mechanical re-inflation to maintain chest inflation during prolonged breath-holds for radiotherapy
Michael Parkes,
The Netherlands
PO-1072
Abstract
Mechanical re-inflation to maintain chest inflation during prolonged breath-holds for radiotherapy
Authors: Michael Parkes1, Irma Van Dijk1, Jeffrey Veldman1, Zdenko Van Kesteren1, Markus Stevens2, Geertjan Van Tienhoven1, Joost Van Den Aardweg3, Stuart Green4, Thomas Clutton-Brock5, Arjan Bel1
1Academic Medical Centre (AMC), Department of Radiation Oncology, Amsterdam, The Netherlands; 2Academic Medical Centre (AMC), Anaesthesiology, Amsterdam, The Netherlands; 3Academic Medical Centre (AMC), Lung diseases, Amsterdam, The Netherlands; 4University Hospitals Birmingham, Medical Physics, Birmingham, United Kingdom; 5University Hospitals Birmingham, Critical Care Medicine, Birmingham, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
During
all breath-holds, the chest slowly deflates by ~250 ml/min. During single prolonged
breath-holds of > 5 min., this causes the left breast to move linearly at 2 mm/min.
(± 0 standard error) dorsally (Parkes et al., 2016) and the diaphragm to move linearly at 3 mm/min.
(range 1-5mm) cranially (van Dijk et al., 2021). When using such prolonged
breath-holds for radiotherapy, this would alter tumour position. Here we
studied whether the mechanical ventilator can be used to re-inflate the chest during
the breath-hold. Simply applying continuous inflation during breath-holding is
ineffective because the larynx may close. Instead, we tested here whether subjects
could be instructed at intervals to attempt a minimal inhalation using their
diaphragm. This could trigger the ventilator to superimpose a constant
inflation of short duration. The net effect of these short inflations should be
to maintain the chest inflated until the breakpoint (i.e., to have abolished the slow deflation).
Material and Methods
Single
prolonged breath-holds of > 5 min. were induced by mechanical hyperventilation
and preoxygenation (Parkes et al., 2016) with Hamilton MR1 or T1 non-invasive
ventilators in 8 healthy volunteers. In 5, chest circumference was measured continuously
with a wrap-around band connected to a spring-loaded resistor. In 3 others,
diaphragm position was measured in the MRI using a 1D navigator acquisition at
2 Hz frequency.
Results
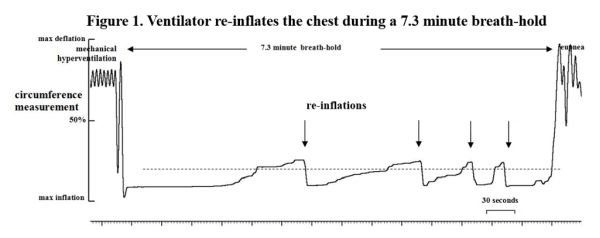
During
single prolonged breath-holds in 5 subjects
( mean duration 7 min. (±1 se min)), they were instructed to attempt a
minimal inhalation each time deflation had reached an arbitrary threshold level.
This enabled the chest to remain at the inflation circumference at breakpoint
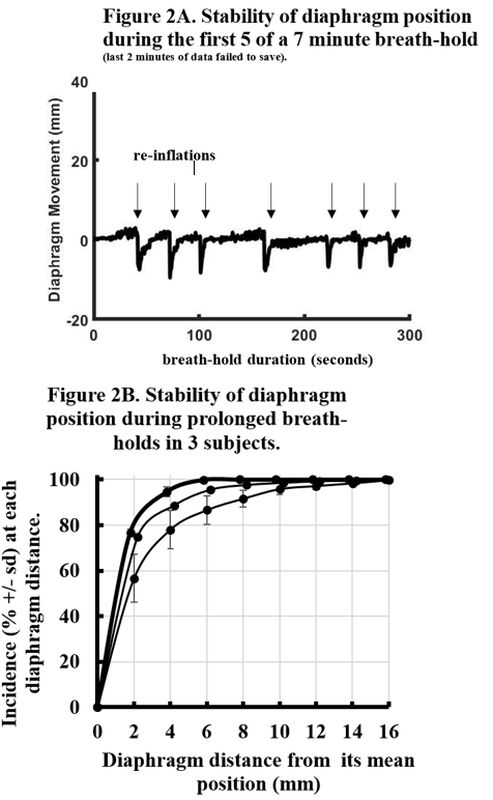
(figure 1). During prolonged breath-holds in 3 subjects (mean duration 6 min. (± 1), they were instructed to attempt a
minimal inhalation once or
twice every minute (figure 2a). Here, while the diaphragm briefly descended and re-ascended by ~5 mm during each inhalation, for ~90% of time the diaphragm position
remained stable within 4 mm of its mean position (figure 2b). At breakpoint the
diaphragm was within 3 ± 1 se mm of
its starting position.
Conclusion
We
demonstrate how instructing healthy volunteers to perform this manoeuvre can
overcome the deflation that normally occurs during all breath-holds. Training
patients with thoracic or abdominal tumours to perform this manoeuvre during
prolonged breath-holds could prevent the chest deflating. This could reduce
tumour movement during, and increase the usable breath-hold duration available
for radiotherapy treatment.
Parkes MJ, et al., (2016) B J Radiol 89, 20160194.
van Dijk
IW et al., (2021) ESTRO OC-0339.