Radiotherapy Quality Assurance; is volume review all that matters?
Maeve Keys,
United Kingdom
PO-1071
Abstract
Radiotherapy Quality Assurance; is volume review all that matters?
Authors: Maeve Keys1, William Croxford1, Chaya Fligg2, Anna France3, Cy Howells3, Ed Smith1, Shermaine Pan1
1The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom; 2Manchester University, Medicine, Manchester, United Kingdom; 3The Christie NHS Foundation Trust, Proton Clinical Outcomes Unit, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
RTQA practice is known to have significant variation amongst
institutions worldwide. It is critical to maintaining patient safety, treatment
effectiveness and accuracy. However there is no standard practice, with often
only target volume delineation reviewed alone and performed retrospectively. Previous
studies have highlighted higher rates of changes made in more complex
techniques and subsites. This study aims at evaluating our prospective structured
peer review process in a proton beam therapy (PBT) centre.
Material and Methods
We reviewed the RTQA cases of all patients treated at The
Christie Proton Beam Centre since its opening in November 2018 until February
2021. The RTQA process is carried out weekly, is subsite specific and every
case has their target volumes and plans reviewed in detail in the presence of
consultants, fellows, physicists and dosimetrists. Since the COVID-19 pandemic,
the peer review meetings are now virtual. Every peer review has a standardised
RTQA form filled. We classified the peer reviews as having major/minor or no
change. A major change was one where the target volumes (GTV and/or CTV) were
too small or big; dose fractionation was incorrect to that of the prescription
treated and any plan that was changed. A
minor change was one where there were minor modifications to the target volumes,
OARs or non-essential suggestions in relation to the plan that didn’t result in
the plan being altered eg. addition of an OAR.
Results
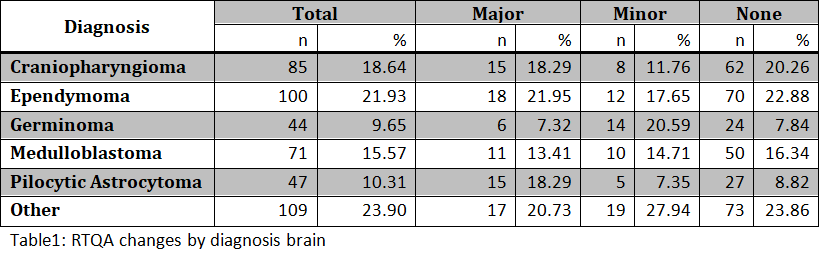
There was a total of 1,209 peer reviews for 462 patients. 100% of cases had both volumes and plans peer reviewed prospectively. 591 were reviews of target volumes and 618 were plan reviews. In total there were 208 (17%) major changes, 194 (16%) minor and 807 (67%) with no changes. Of the major changes 137 (66%) were target volumes and 71 (34%) plans. Of the minor changes 174 (90%) were target volumes and 20 (10%) plans. There were more major and minor changes in the brain and head & neck subsites possibly due to their complexity. When diagnoses in the brain were categorised (Table 1) and reviewed against changes using a chi-squared test the resulting p-value = 0.027 suggests a significant relationship between type of diagnoses and likely need for change following peer review.
Conclusion
Target volume delineation and radiotherapy plans
particularly in brain, head & neck as well as other complex subsites require
mandatory prospective review as highlighted above. We have shown this to be
practically achievable and successful despite challenging times.