Quantitative benefit of centralised quality assurance for the implementation of Lung SABR
Mariana Kroiss,
United Kingdom
PO-1030
Abstract
Quantitative benefit of centralised quality assurance for the implementation of Lung SABR
Authors: Mariana Kroiss1, Rushil Patel1, Patricia Diez1
1Radiotherapy Trials Quality Assurance Group, Mount Vernon Cancer Centre, Radiotherapy Physics, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
SABR has become standard of care for early
stage lung cancer where surgery is contraindicated. As a result of the COVID-19
pandemic access to surgery was limited and demand for SABR as primary treatment
has increased. A national program to implement
lung SABR in all radiotherapy centres was commissioned and an associated QA program
was developed. One of its components was a planning benchmark case to ensure optimal
planning of target volumes whilst sparing organs at risk following the SABR
Consortium Guidelines.
Results of the benefits of the QA process are presented here.
Material and Methods
A dual-lesion planning benchmark DICOM
dataset was circulated amongst 24 participating centres, including a planning
CT and a structure set. Centres had to plan the lesions to 55Gy in 5# and meet
dose constraints, coverage and conformity criteria outlined in the Guidelines. All plans were reviewed on Velocity v4.1
(Varian Medical Systems) and PTV coverage, dose distribution, plan conformity
and OAR dose constraints were assessed. Prescription Dose Spillage (PDS) was
used to define conformity in the high dose area as Body V100(cc)/PTV V100(cc) and Modified Gradient Index (MGI) was
defined for conformity in low dose area as Body V50(cc)/PTV V100(cc). The
Mann Whitney test was used to evaluate differences in conformity across plans,
with statistical significance set at 5%.
Results
Mean
V100% for first submissions for lesions 1 and 2 were 97.26% (S.D.
1.86) and 98.19 % (S.D.1.61), respectively. All mandatory OARs were well within
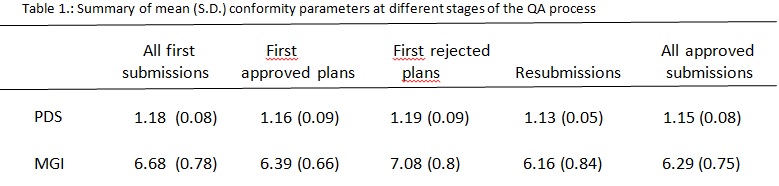
tolerance. The largest variation across centres was plan
conformity, which is summarised in Table 1.
Ten
plans failed their first attempt and centres were asked to resubmit following
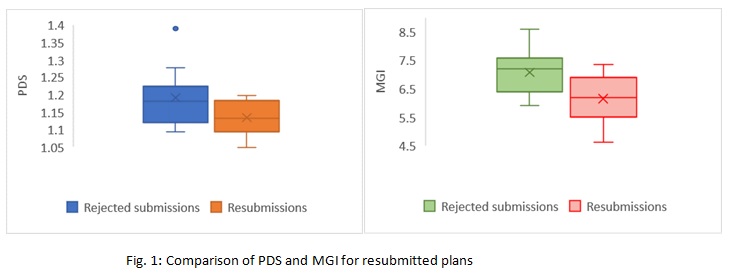
detailed feedback. Mean PDS for these
plans changed from 1.19 (S.D. 0.09) to 1.13 (S.D. 0.05), although this was not
statistically significant (p=0.12). Mean MGI was significantly improved on resubmission,
decreasing from 7.08 (S.D. 0.8) to 6.16 (S.D.0.84), (p=0.03).
Figure 1 shows increase in consistency and improvement in conformity across
centres after resubmission. On completion of the QA process, the final set of
accepted plans had improved conformity indices from initial PDS and MGI,
however these were not statistically significant (p=0.31 and p=0.13, respectively).
Conclusion
A national QA program for lung SABR is critical
for the safe implementation of this technique and to ensure standards are consistently
high across multiple centres. The planning benchmark has highlighted
differences in plan conformity and technique, in particular for MGI, however
feedback within the QA process has allowed for increased consistency across
departments through improved quality.