97 patients with anal cancer were identified, of which 44 were PLWH. Complete CBC counts were available for 90 patients. Radiation therapy was commonly prescribed to 50.4-54 Gy using IMRT; 3 patients underwent RT alone (all PLWH); Chemotherapy was 5-FU+Mitomycin-c (34 HIV-/27 PLWH), Capecitabine+Mitomycin-c (16 HIV-/11 PLWH), or other (3 HIV-/3 PLWH).
Median follow-up was 55 months in HIV- patients (rg: 10-150) vs. 59 months in PLWH (rg: 5-164). Among HIV- patients there were 45% stage I/II and 55% stage III, in PLWH there were 40% stage I/II and 60% stage III. There were 10/53 vs. 7/44 loco-regional recurrences in the HIV- vs. PLWH group, 9 vs. 2 distant metastases, and 9 deaths in both. Outcomes (HIV- vs. PLWH) were comparable with 2‑year PFS at 76.9% vs. 83.8% (p=.40) and OS at 92.3% vs. 92.8% (p=0.93). Substitution of 5-FU with capecitabine had no effect on outcomes in either group (p>0.73).
G3+ Lymphopenia occurred in 83% (n=44) vs. 89% (n=32) (p=.35), G3+ neutropenia occurred in 21% (n=11) vs. 56% (n=20) (p<.01), and G3+ thrombocytopenia occurred in 8% (n=4) vs. 33% (n=12) (p<.01) of patients in the HIV- and PLWH groups, respectively. Absolute ABM V5Gy to V40Gy was associated with delayed recovery in platelet counts for HIV- (0.40‑0.56; p≤.04) and PLWH (0.41; p=.04) patients (Fig.1), with a sharp increase at volumes above 275cm3 (HIV-) and 350cm3 (PLWH), while rel. V5Gy (-0.29; p<.04) for HIV- and abs. V5Gy to V40Gy (-0.43; p≤.02) for PLWH were associated with a more rapid drop in lymphocytes showing no threshold (Fig.2).
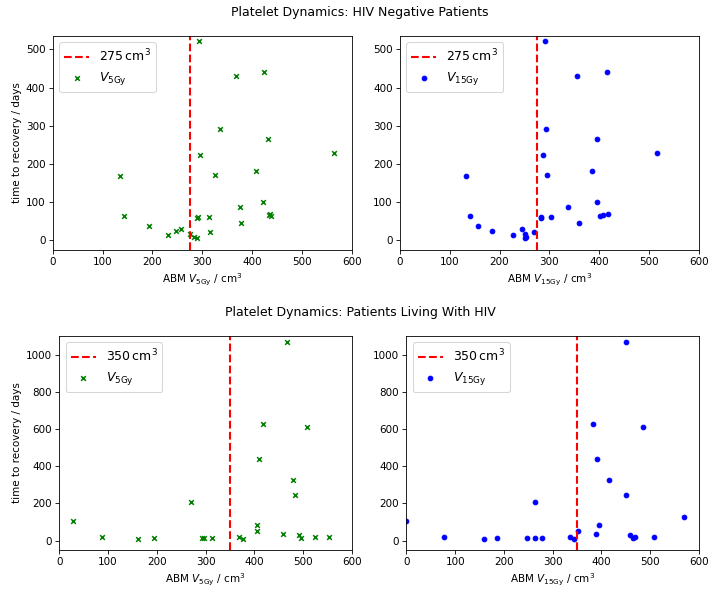
Figure 1. Time to recovery association with ABM V5Gy and V15Gy.
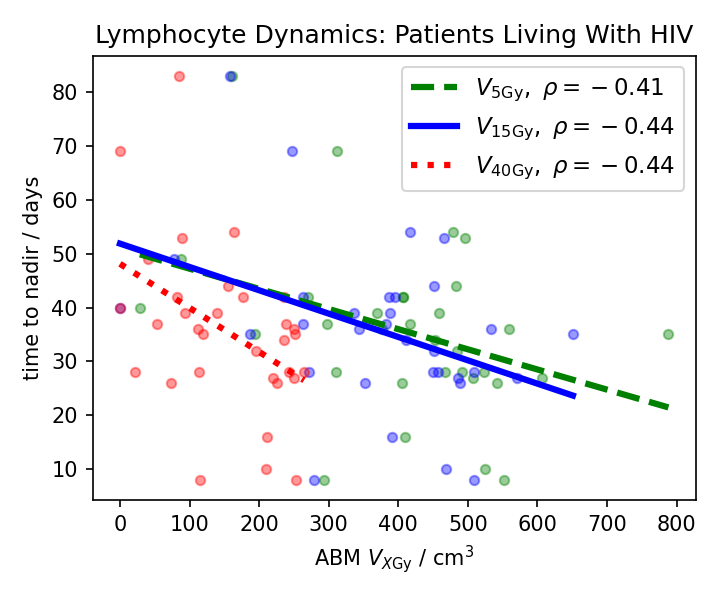
Figure 2. Time to nadir association with volumetric ABM dose metrics.