Stereotactic MR-guided Adaptive RT for rectal cancer: toxicity, radiological & pathological response
Alessandra Castelluccia,
Italy
PD-0495
Abstract
Stereotactic MR-guided Adaptive RT for rectal cancer: toxicity, radiological & pathological response
Authors: Alessandra Castelluccia1, Domenico Marchesano1, Gianmarco Grimaldi2, Ivan Annessi1, Federico Bianciardi1, Cristian Borrazzo1, Annamaria Di Palma1, Randa El Gawhary1, Marica Masi1, Maria Rago1, Maria Valentino1, Laura Verna1, PierCarlo Gentile1,2
1San Pietro Fatebenefratelli Hospital, Radiation Oncology, Rome, Italy; 2UPMC San Pietro FBF, Radiation Oncology, Rome, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Short-course
irradiation reduces the risk of local recurrence and showed overall survival improvement
with a lower rate of early toxicity when compared to chemoradiation. Previous
studies demonstrated that radiotherapy dose of neoadjuvant treatments is a significant predictor of achieving a
local response. The purpose of this
study is to measure the effects of stereotactic MR-guided adaptive radiotherapy
(SMART) for rectal cancer patients in terms of early toxicity, radiological
and pathological response.
Material and Methods
Patients
diagnosed with local advanced rectal cancer with positive lymph node staging,
resectable (cT3 with > 5 mm extramural invasion and uninvolved MRF) or
unresectable unfit for chemotherapy, underwent
SBRT on rectal lesion and mesorectum with patological nodes using hybrid MR-Linac
(MRIdian ViewRay). Treatment
prescription at 80% isodose for the rectal
lesion and mesorectum with pathological nodes was
40Gy (8Gy/fr) and 25 Gy (5Gy/fr),respectively,
delivered on 5 days (3fr/week). The gross target volume (GTV) was
identified on a true fast imaging (TRUFI) MR scan acquired during simulation
and prior to each fraction to adapt the treatment plan of the day. New plans were calculated
and delivered every fractions because of rectal and bowel motion. An
intrafraction motion management strategy was applied, consisting of a gating
approach based on the real-time acquisition of a sagittal cine MRI during the
whole delivery time (temporal resolution: 8 frames/s). Response assessment by MRI was performed 3 weeks
after SMART, than patients fit for surgery underwent total mesorectal excision.
Adverse effects of RT were
scored according to the NCI Common Toxicity Criteria (CTC) scale, version 5.0.
Results
Twenty patients underwent rectal SMART. No G3-5 toxicity was recorded. A moderate or good
radiological response (mrTRG≤3) was observed in all of this patients. Twelve patients were elegible for total mesorectal excision.
Mean interval between the
completion of SMART and surgery was 4
weeks. Pathological downstaging occurred in all patients, 2 patients achieved complete response (pCR). pCR occured with a
prolonged time to surgery (>7 weeks). Patients
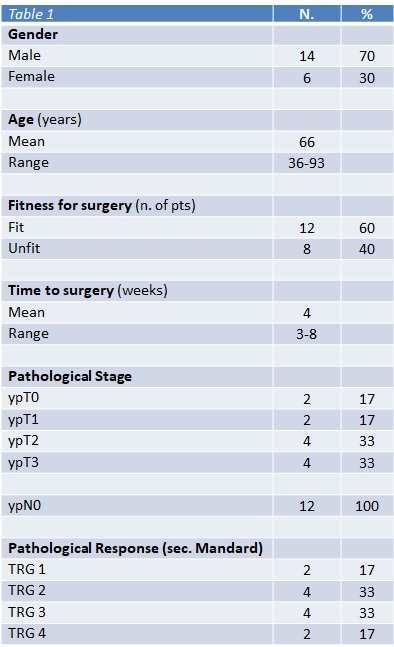
baseline characteristics, pathological stage and response are listed in Table 1.
Conclusion
SMART for
rectal cancer is well tolerated and effective in terms of tumor regression.
This radiation treatment can help to achieve a complete pathological response in selected
patients, especially when followed by delayed surgery. In addition, short-course schedule is less expensive and time saving,
therefore SMART could be useful to treat a larger number of patients and
to reduce patients’ waiting list. However, further studies are required to
confirm these findings.