106 pts were treated: Histology: NSCLC 80/106 (75%), SCLC 21/106 (20%), thymic
malignancies 5/106 (5%). Definitive chemoradiation in 101/106 (95%), or adjuvant
radiation in 5/106 (5%) to mean radiation dose 59.9 Gray delivered in 30 fractions
with VMAT.
13 cases treated concurrent with SBRT to primary lung
lesion that was peripheral to the mediastinal nodal spread.
Indications for DIBH were COPD (11%), large PTV (44%), small
lung volume (10%) prior immunotherapy (IT) (5%), re-radiation (3%), or prior lobectomy
(13%).
Compliance with DIBH was optimal 93% (99/106) completed
treatment. 4 patients were unable to comply with DIBH in the planning CT; 3
cases have begun treatment with DIBH but could not finish (total 7/106, 6.6%,
all female).
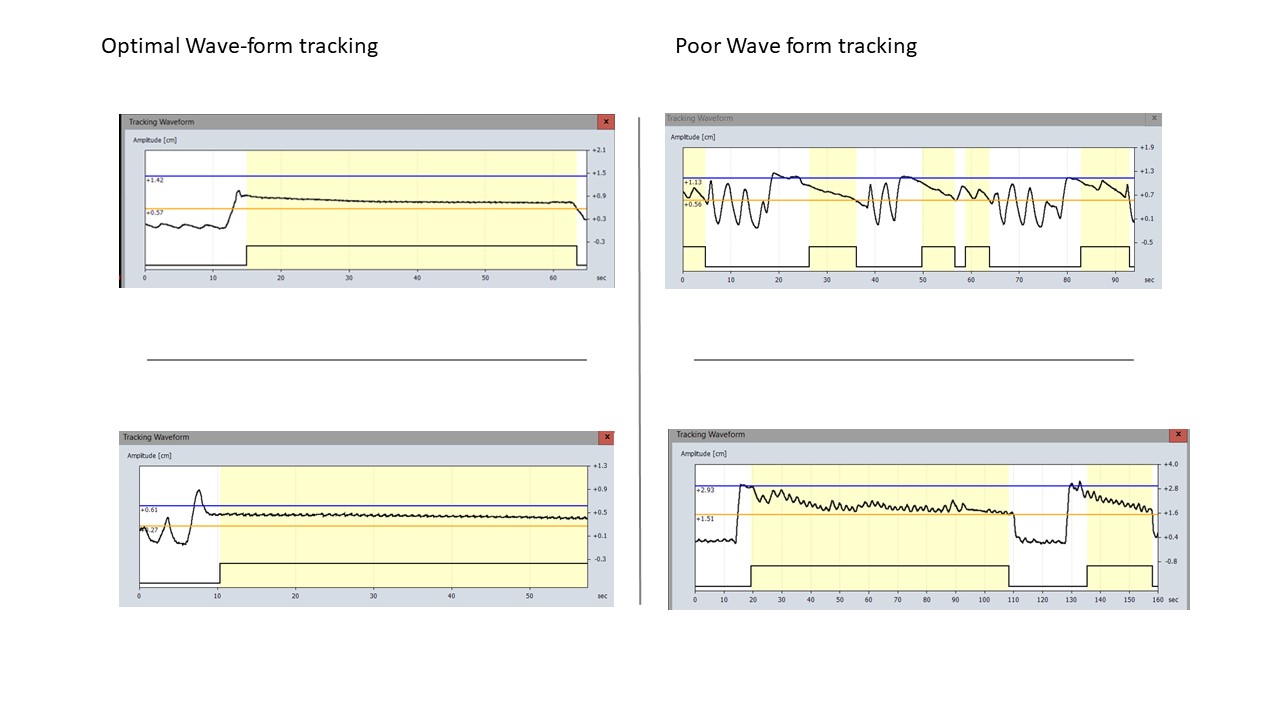
DIBH reproducibility (lung inflation) was reproduced
throughout fractions adequately in 91/102 (89%), satisfactory in 8/102 (8%) but
inadequate in 3/102 (3%).
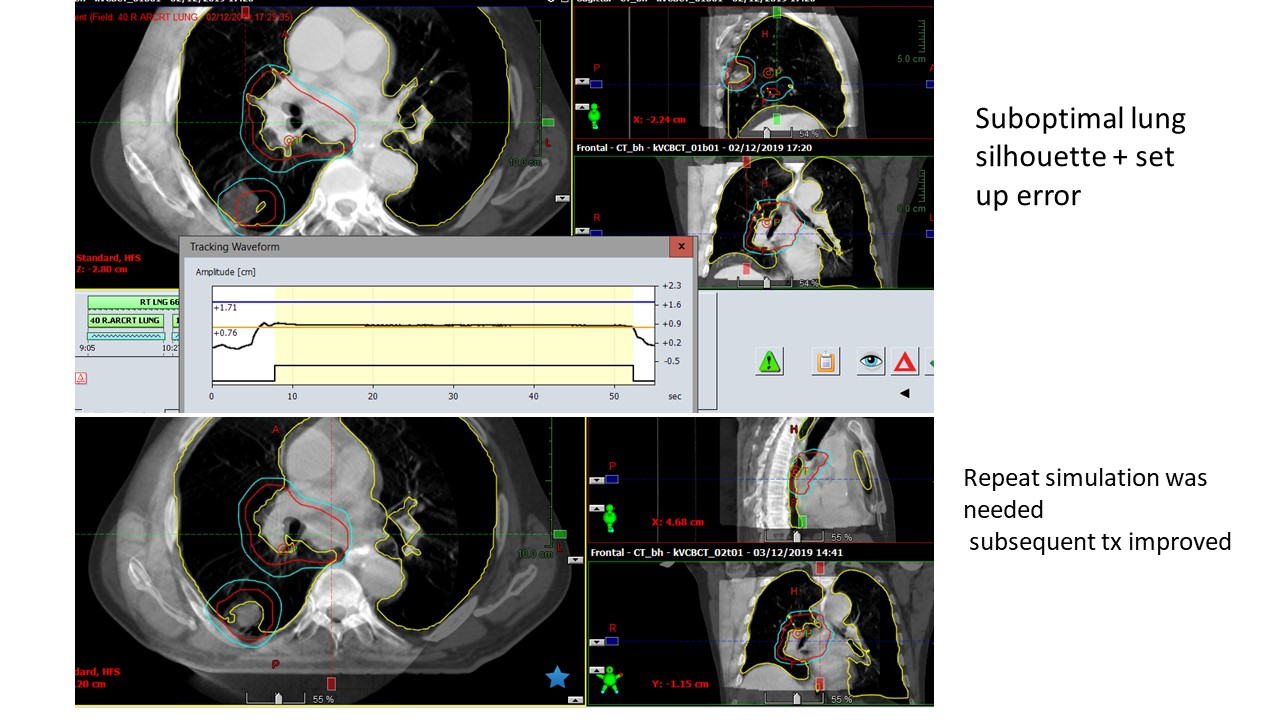
Set up accuracy was perfectly registered to the CTV in
86/102 (84%), adequate (inside PTV) in 13/102 (13%) but inadequate in 3/102 (3%).