Reirradiation in head and neck cancer. Who would benefit? Retrospective analysis of our experience
PO-1203
Abstract
Reirradiation in head and neck cancer. Who would benefit? Retrospective analysis of our experience
Authors: Raquel Granado1, Fabio Pires2, Sergi Benavente2, Marcelino Hermida3, David Sanchez4, Alba de Pablo5, Juan David Assaf6, Irene Braña6, Jordi Giralt1
1Vall d'hebron Hospital, Radiation Oncology, Barcelona, Spain; 2Vall d'hebron Hospital, Radiation Oncology, Barcelona , Spain; 3Vall d'hebron Hospital, Physics, Barcelona , Spain; 4Vall d'hebron Hospital , Physics, Barcelona, Spain; 5Vall d'hebron Hospital, Oral and Maxillofacial surgery, Barcelona, Spain; 6Vall d'hebron Hospital, Medical Oncology, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy (RT) plays a fundamental role in the definitve treatment of squamous cell carcinoma of the head and neck. Despite optimal initial treatment, approximately 30-40% of patients will experience a locoregional relapse or second primary tumour. The management of this presents a major clinical challenge when re-treating an already irradiated field where the balance between the benefit to the patient vs. the risk of toxicity is narrow. With this analysis we aim to provide data to facilitate a rigorous selection and stratification of patients who could benefit from re-irradiation treatment.
Material and Methods
We retrospectively analysed a series of patients with loco-regional relapse or 2nd primary head and neck cancer who were reirradiated between 2009-2021 in a previously irradiated field (≥50Gy) using 3D or IMRT and conventional fractionation. Data on disease-free survival (DFS), overall survival (OS), acute and chronic toxicity are presented.
Results
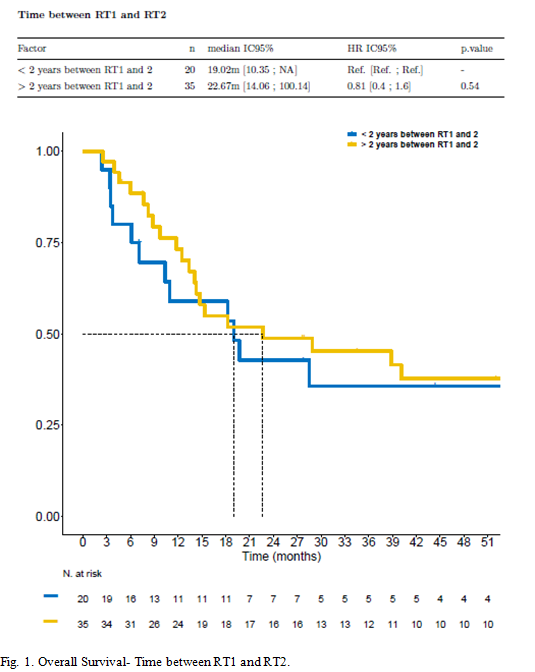
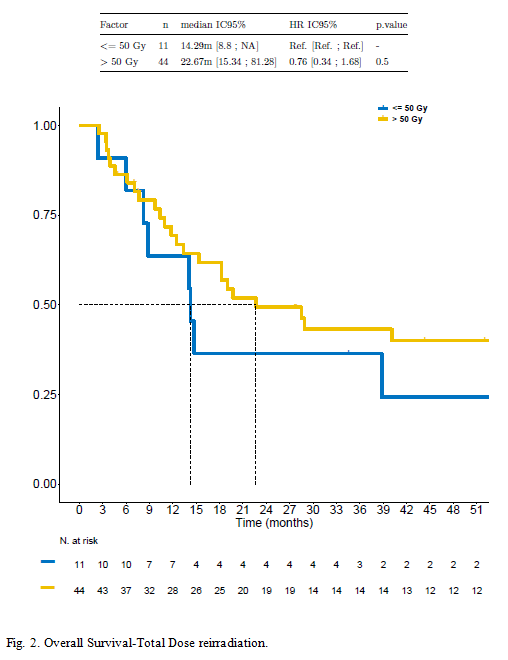
55 patients were analysed. 20 patients (36%) were reirradiated within two years after the first irradiation, 35 (64%) after 2 years and none before 6 months. Almost the entire sample had an ECOG performance status ≤ 1 (n=54) at the time of reirradiation, demonstrating in the multivariate analysis performed that it is related to an improvement of the OS (HR 0.66, CI 0.29-1.52, p=0.33).Figure 1 shows the OS as a function of this time between initial treatment and reirradiation, showing a positive trend when the retreatment time is longer than 2 years, although it does not show statistical significance. The most frequent location was the oral cavity (n=21, 39%). Most of them underwent adjuvant RT (n=32, 58%), reaching a mean dose of 59.95Gy (70.00-48.40) in addition to concomitant chemotherapy (67%). As we can see in figure 2 OS increase at doses above 50Gy. Regarding toxicity, the most frequent was acute toxicity (95%) in terms of mucositis and dermatitis G1-G2 according to the CTCAE v4.0 scale, 49% and 60% respectively. The incidence of chronic toxicity was 74%, with 9% G3-G4 trismus, 6% G3-G4 osteoradionecrosis and 36% G3-G4 dysphagia of which, 28% of the patients required gastrostomy placement due to RT. The Median DFS after completion of reirradiation was 4.7 months (range 1-110) and median OS after reirradiation was 17.1 months (1-130).
Conclusion
In view of our results we can conclude that in patients undergoing radical or adjuvant re-irradiation treatment, time between first and second irradiation longer than two years, good performance status and doses higher than 50Gy improve results.