Elective node irradiation and perineural invasion in salivary gland tumors: the MedAustron approach
Ankita Nachankar,
Austria
PO-1178
Abstract
Elective node irradiation and perineural invasion in salivary gland tumors: the MedAustron approach
Authors: Ankita Nachankar1,3, Eugen Hug1, Petra Georg1, Maciej Pelak1, Slavisa Tubin1, Joanna Gora2, Astrid Fraller1, Petra Mozes1, Piero Fossati1,4
1MedAustron Ion Therapy Center, Austria, Radiation Oncology, Wiener Neustadt, Austria; 2MedAustron Ion Therapy Center, Austria, Medical Physics, Wiener Neustadt, Austria; 3ACMIT Gmbh, Austria, Research and Development in Medical Technology, Wiener Neustadt, Austria; 4 Karl Landsteiner University of Health Sciences, Austria, Radiation Oncology, Krems an der Donau, Austria
Show Affiliations
Hide Affiliations
Purpose or Objective
Purpose: Salivary gland cancers (SGCs) are uncommon malignancies with unique biology and natural course. In non resectable cases outcomes with photons-based RT or RT-CHT remain suboptimal as compared to squamous cell carcinoma. Carbon ions have shown promising results in non-resected SGCs in German and Japanese studies. In the German experience elective nodal irradiation (ENI) was routinely used in clinically node negative (cN0) SGCs, however Japanese centers never performed ENI and isolated neck recurrence were rare in their series. There is no consensus on need of ENI in SGCs. Perineural invasion (PNI) is at least as important as lymphatic spread in SGC. Risk of lymph node involvement and PNI in SGCs is highly variable across histologies, primary site and T stage. Here we propose recommendations for clinical target volume (CTV) with respect to ENI and PNI in cN0 SGCs.
Material and Methods
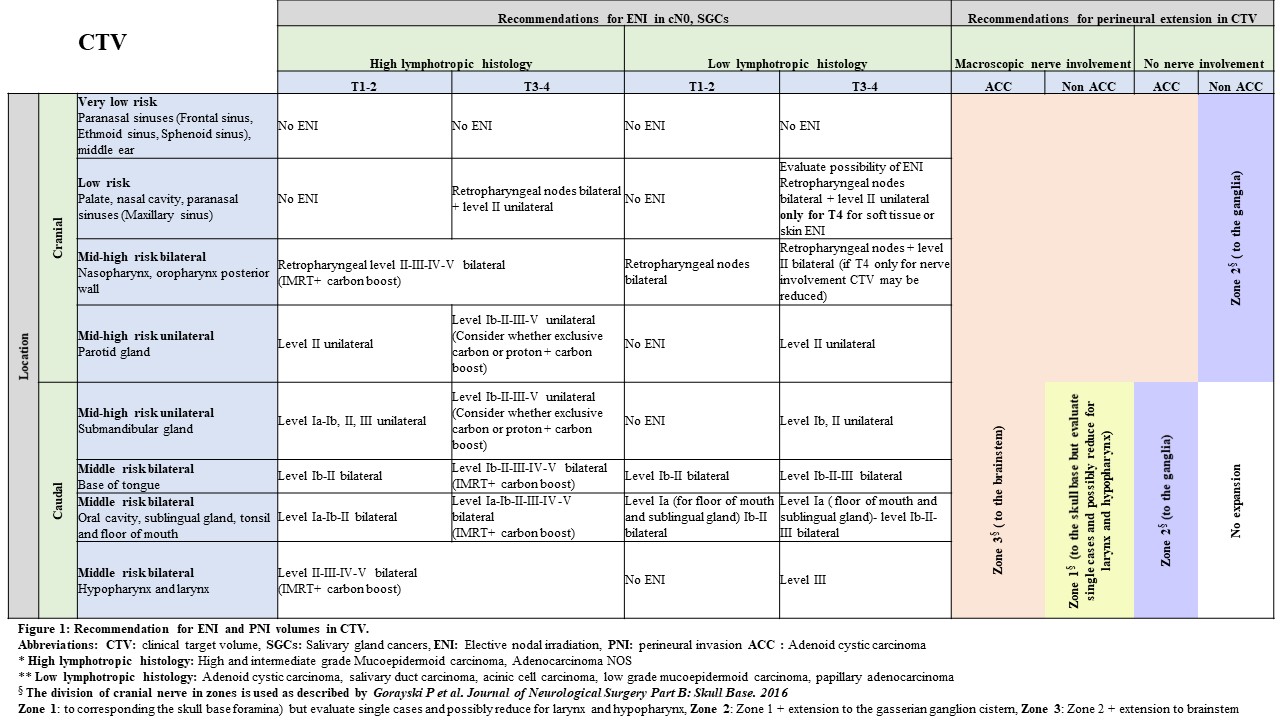
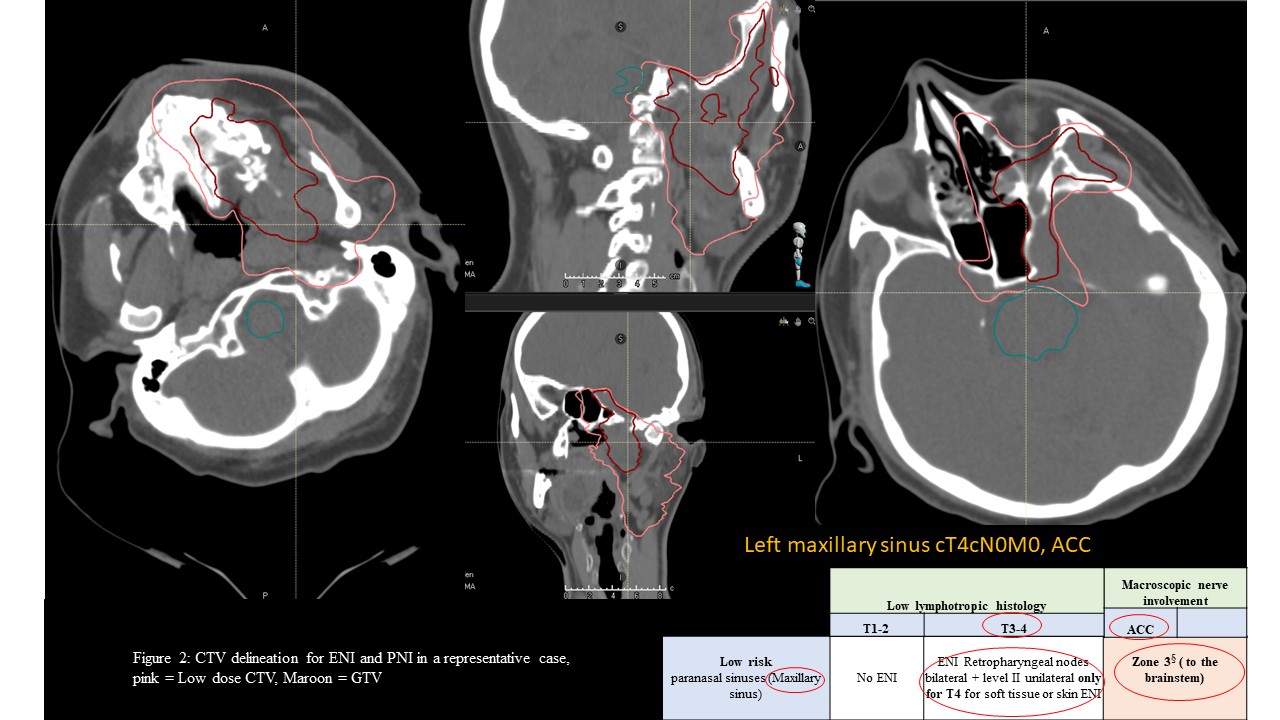
Material/Methods: We stratified cN0, SGCs as per T stage, primary site and histologies. For ENI Tumor locations were classified into, very low risk, low risk, mid-high risk unilateral and mid-high risk bilateral groups for lymphatic spread (figure 1). SGC histologies were divided into highly lymphotropic- high and intermediate grade mucoepidermoid carcinoma, adenocarcinoma NOS and low lymphotropic- Adenoid-cystic carcinoma (ACC), salivary duct carcinoma, acinic-cell carcinoma, low grade mucoepidermoid carcinoma, papillary adenocarcinoma (figure 1).
For PNI, tumors were grouped into cranial and caudal primary site (figure 1, 2) and ACC were classified as neurotropic and non-ACC as non-neurotropic histologies. Twenty-three patients with SGCs treated with CIRT +/- proton therapy at MedAustron from July 2019 to September 2022 were analysed. Prescription dose CIRT (n =20) was 57 .6 - 70.5 Gy [RBE]/12 -22 fractions, with 4-5 fractions/ week. Three patients received proton therapy 50-54 Gy [RBE]/ 25-27 fractions followed by CIRT boost 12- 20 Gy [RBE]/4-5 fractions, with 4-5 fractions/ week.
Results
Results: Median follow up was 12.2 months (range, 2.5 – 36.3). Majority of patients had advanced T stage; 1 patient had positive node at surgery. ACC was most common histology followed by mucoepidermoid carcinoma, and pleomorphic adenoma. PNI were evident in 13 patients at baseline and 1 patient developed postop facial paralysis. Two (2/23) patients had local progression, none had nodal or distant failure. 1- and 2-year loco-regional control rate is 95.7%, 81.3% respectively. Two (2/23) patient developed acute grade 3 mucositis and 1 developed grade 3 dermatitis; none developed grade >/= 3 late toxicity.
Conclusion
Conclusion: Isolated nodal failure in cN0, SGCs are very rare. This work can be considered a first step toward creating a consensus on ENI and PNI volumes in this population.