Outcomes in oropharyngeal squamous cell carcinomas based on gross tumour volume
PO-1175
Abstract
Outcomes in oropharyngeal squamous cell carcinomas based on gross tumour volume
Authors: Darragh Browne1, Orla McArdle2, Emma Connolly2, Megan McNamara2, Jane Burns2, Mary Dunne3
1St Luke's Radiation Oncology Network, Radiation oncology, Dublin, Ireland; 2St Luke's Radiation Oncology Network, Radiation Oncology, Dublin, Ireland; 3St Luke's Radiation Oncology Network, Biostatistics, Dublin, Ireland
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the prognostic significance of gross tumour volume (GTV) (primary and nodal) as well as other variables in patients with oropharyngeal squamous cell carcinoma (OPSCC) treated with radiation therapy (RT) in a single centre in Ireland.
Previous work by Adrian et al. demonstrated that primary GTV predicted both recurrence and overall survival. In the current study we investigate if this is replicated in the Irish setting, and also if nodal GTV predicts for outcome.
Material and Methods
- Data were collected retrospectively on 139 patients treated with curative RT for OPSCC in the St Luke’s Radiation Oncology Centre, Beaumont Hospital from 2013 to 2021.
- TNM 8th edition definition of stage was applied.
- Descriptive statistics, survival and cox regression analyses were performed using R v4.2.1 (Copyright (C) 2022 The R Foundation for Statistical Computing).
Results
Of 139 patients, median age was 59.4, 102 (73.4%) were male, 102 (73.4%) had p16+ disease, and 116 (83%) received concomitant chemotherapy. Median follow up was 24 months (0 - 96).
Patients with p16- disease had a more advanced stage at diagnosis (35 (94.6%) had stage 3 or 4 disease), in comparison to their p16+ counterparts (94 (92.2%) with stage 1 or 2 disease). Patients with p16- disease had larger primary GTVs (median 21.8cm3 versus 14.7cm3 in the p16+ cohort) and smaller nodal GTVs (median 6.35cm3 versus 15.75cm3 in the p16+ cohort).
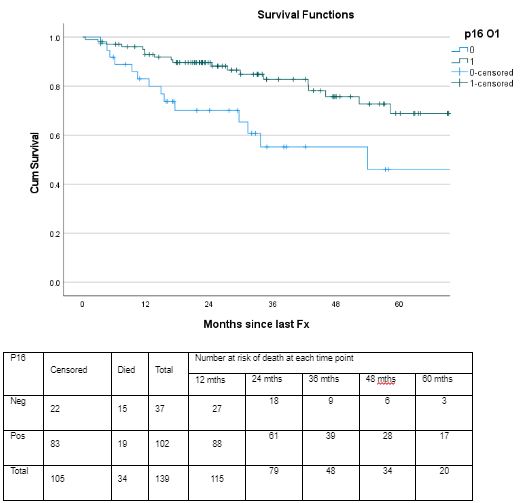
P16 status predicted for both recurrence (p<.005) and survival (p=.015). Median recurrence-free survival was 30 months (95%CI: 6–54 months) for p16- patients. Median recurrence-free survival was not reached for p16+ patients. Median survival was 54 months (95%CI: 36–72 months) for p16- patients. Median survival was not reached for p16+ patients. Stage predited for recurrence (p<.0005) but not survival. Use of concomitant chemotherapy did not predict recurrence (p=.748) or survival (p=.550).
On univariate analysis, both primary and nodal GTV predicted for overall survival (HRs (CI): 1.039 (1.023 - 1.054) and 1.007 (1.002 - 1.012), respectively). On multivariate analysis, primary GTV remained significant in predicting survival (HR: 1.036, CI 1.019 - 1.052).
Conclusion
Primary GTV predicts overall survival in patients with OPSCC treated with RT. This is a measure readily available to Radiation Oncologists at treatment planning, and in the future may aid treatment de-escalation decision making. Further work is needed to identify patients for whom RT can be safely de-escalated, to reduce long term treatment morbidity.
References:
Adrian, G., Carlsson, H., Kjellén, E. et al. Primary tumor volume and prognosis for patients with p16-positive and p16-negative oropharyngeal squamous cell carcinoma treated with radiation therapy. Radiat Oncol 17, 107 (2022).