Sarcopenia in oropharyngeal cancer treated with curative radiotherapy: time for a tailored approach?
PO-1172
Abstract
Sarcopenia in oropharyngeal cancer treated with curative radiotherapy: time for a tailored approach?
Authors: Luca Bergamaschi1,2, Mattia Zaffaroni1, Maria Giulia Vincini1, Giulia Marvaso1,2, Stefania Volpe1,2, Francesca Colombo1,2, Cecilia Bonfiglio1, Stefano Zorzi3, Maria Cossu Rocca4, Annarita Sabbatini5, Giulia Cannillo5, Emanuela Zagallo5, Mohssen Ansarin3, Roberto Orecchia1, Daniela Alterio1, Barbara Jereczek-Fossa1,2
1European Institute of Oncology IRCCS, Division of Radiation Oncology, Milan, Italy; 2University of Milan, Department of Oncology and Hemato-Oncology, Milan, Italy; 3European Institute of Oncology IRCCS, Division of Otolaryngology and Head and Neck Surgery, Milan, Italy; 4European Institute of Oncology IRCCS, Department of Medical Oncology, Urogenital and Head and Neck Tumors Medical Treatment, Milan, Italy; 5European Institute of Oncology IRCCS, Dietetic and Clinical Nutrition Unit, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To identify patients at higher risk of developing sarcopenia during RT and to evaluate the impact on oncological outcome and toxicity profile in a retrospective series of oropharyngeal cancer patients treated with curative RT +/- chemotherapy at a single institution.
Material and Methods
Oropharyngeal SCC patients who underwent curative RT with a prescription of 70 Gy with VMAT technique +/- chemotherapy from 2012 to 2019 were considered for study inclusion. Contouring of the cross-sectional area (CSA) of the masticatory muscles (MM-CSA) at the level of bilateral mandibular notches (Fig.1) and of the paravertebral and sternocleidomastoid muscles at the level of the third cervical vertebra (C3-CSA) (Fig.2) on both simulation and 50 Gy revaluation CT scans was performed. MM-CSA and C3-CSA were used to estimate the CSA at 3rd lumbar vertebra (L3) from validated algorithms, to detect skeletal muscle index (SMI) and consequently assess sarcopenia both at baseline and at 50 Gy, based on predetermined thresholds.
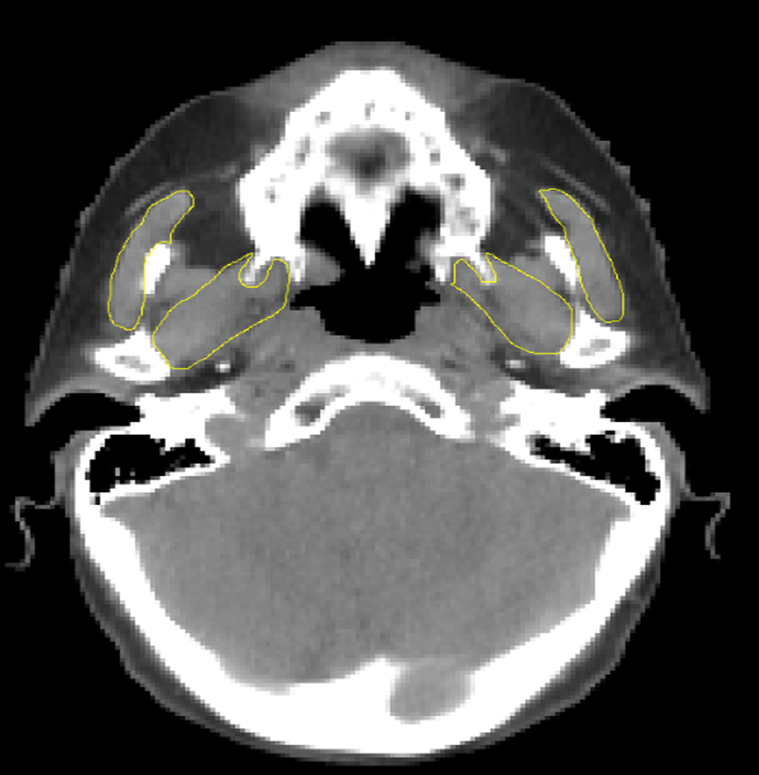
Figure 1 ImageJ delineation of the masticatory muscles (threshold setting: -29 to +150 HU) in a sarcopenic patient.
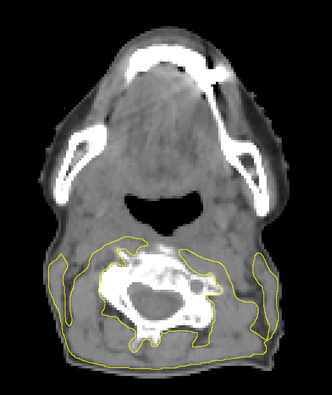
Figure 2 ImageJ delineation of the paravertebral and sternocleidomastoid muscles at the level of the third cervical vertebra (C3) (threshold setting: -29 to +150 HU) in a sarcopenic patient.
Results
One hundred and sixteen patients were included in the study. Most of them had locally advanced (95.7%) and HPV-associated carcinomas (74.1%) and were treated with concurrent chemotherapy (90.5%). Based on MM-CSA, becoming sarcopenic during RT (16 patients) was associated with worse PFS (HR 2.52, 95% CI 1.09-5.83, p = 0.03) on multivariate analysis and a trend of correlation with OS was evident too (HR 2.69, 95% CI 0.99-7.28, p = 0.05). Based on C3-CSA, becoming sarcopenic during RT (14 patients) was associated with worse PFS (p = 0.0096) and OS (p = 0.013) on univariate analysis; these correlations were not confirmed on multivariate analysis. Based on both MM-CSA and C3-CSA, no statistically significant associations were found between sarcopenia and worse RT toxicity. Based on C3-CSA, a statistically significant association was present between becoming sarcopenic during RT and reduced baseline haemoglobin values (p = 0.03) and the activation of nutritional counselling during RT (p = 0.02).
Conclusion
Our data suggest that early identification of sarcopenia during RT could bring additional information to aid clinical decision making i.e., the activation of a prompt nutritional intervention to improve oncological outcomes. Further research with prospective trials, especially in HPV-associated oropharyngeal carcinoma, is needed to identify valid biomarkers and better include sarcopenia in a tailored approach to these patients with long life expectancy, involving, for example, the implementation of more sophisticated technologies, such as proton-therapy.