Deep learning-based IMRT treatment planning on synthetic-CT for ART in NSCLC-patients
PO-1637
Abstract
Deep learning-based IMRT treatment planning on synthetic-CT for ART in NSCLC-patients
Authors: Dylan Callens1,2, Liesbeth Vandewinckele2, Patrick Berkovic1, Frederik Maes3,4, Maarten Lambrecht1,2, Wouter Crijns1,2
1UZ Leuven, Department of Radiation Oncology, Leuven, Belgium; 2KU Leuven, Laboratory of Experimental Radiotherapy, Leuven, Belgium; 3UZ Leuven, Medical Imaging Research Center, Leuven, Belgium; 4KU Leuven, Processing Speech and Images (ESAT/PSI), Leuven, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients with NSCLC-tumours could benefit from adaptive radiotherapy. To increase the efficiency of an adaptive workflow, daily CBCT-imaging could be used for treatment planning. Our group reported on CT-based treatment planning by autoplanning for lung IMRT using DL-based fluence map generation. This work investigates the performance of this treatment plan prediction on acquired CBCT images. The CBCT images are converted to syntheticCT’s (sCT) utilising two separate commercial solutions. The generated treatment plans are compared with semi-automatic planning created on the sCT’s.
Material and Methods
For this retrospective study, 9 NSCLC-cases were selected out of a recent database of stage III/IV-patients. These cases were chosen upon fractionation scheme (60/66Gy in 30/33Fx). The mid-treatment CBCT was non-rigidly registered with planningCT to create sCT’s. Deformations were done in MIM and Velocity. Target structures of planningCT were deformed accordingly. Syngo.via was used to autocontour OAR. Three independently fluence-prediction networks with different inputs (deformed structures [RS]; sCT; initial beam dose, rigidly transformed [D]) delivered fluences used for dose computations of the DL-based plans in Eclipse TPS. Semi-automatic planning through RapidPlan mimics standard-of-care planning workflow. All plans started from an in-house IMRT class-solution with 9 beams. Plan- and DVH-parameters were used for plan comparison.
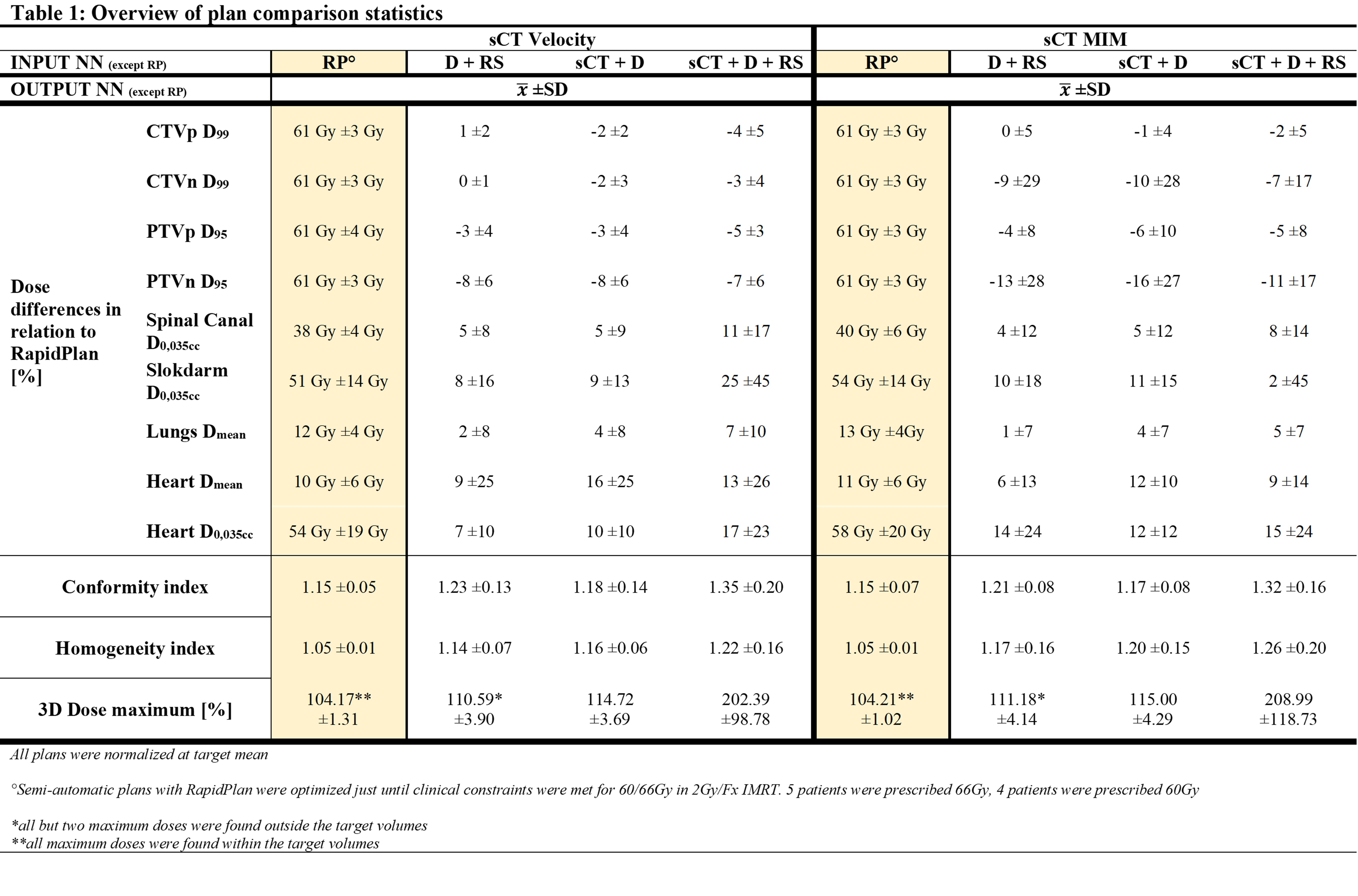
Results
Both sCT’s could be used to generate structures necessary for the clinical standard planning as well as the fluence prediction. The current planning workflow outperformed fluence prediction meeting all clinical constraints. In this case, dose maximums, HI- and CI-values were similar on both sCT’s. In total, 12 of 54 DL-plans met all DVH-constraints. DL-based planning often resulted in an inferior coverage of PTV and a higher dose on OAR. Inferior coverages occurred mainly when visible tumor deformation was observed. MIM noticeably deformed more than Velocity, although both transformation models are accompanied with uncertainty in truthfulness of deformation. Input for the networks is of influence. The combination D+RS led to plans with higher target coverage together with lower doses on OAR and equally acceptable HI/CI, in comparison with other inputs. The combination sCT+D+RS as input resulted repeatedly in unacceptable plans due to a high hotspot outside targets.
Conclusion
Our in-house DL-based planning solution based on fluence prediction has potential to be used for ART on sCT+D or D+RS as input. However, in most cases, it led to plans with higher doses on OAR and underdosage on PTV in comparison with current planning. The AI-model seems to be focusing more on the relation between initial beam dose and corresponding fluence maps but investigating this in-depth is required. Furthermore, the need for better CBCT-imaging is essential for improved veracity of the actual anatomy. By this, we can avoid using sCT’s and eliminate associating uncertainties.