corneal surface reconstruction and pupil tracking for eye localization in ocular proton therapy
Riccardo Via,
Switzerland
MO-0958
Abstract
corneal surface reconstruction and pupil tracking for eye localization in ocular proton therapy
Authors: Riccardo Via1, Giovanni Fattori1, Alessia Pica1, Guido Baroni2, Antony Lomax1, Damien Charles Weber1, Jan Hrbacek1
1Paul Scherrer Institute, Center for Proton Therapy, Villigen, Switzerland; 2Politecnico di Milano, Dipartimento di Elettronica, Informazione e Bioingegneria, Milano, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
We present a customised optical system that combines pupil tracking with corneal topography for non-invasive eye localisation. The system performance was compared to the current clinical protocol which makes use of X-ray imaging of tantalum clips sutured to the patient’s eye. In this study, the system was tested for use in MR-based ocular proton therapy, an envisioned non-invasive protocol that uses MRI imaging to create a patient-specific eye model.
Material and Methods
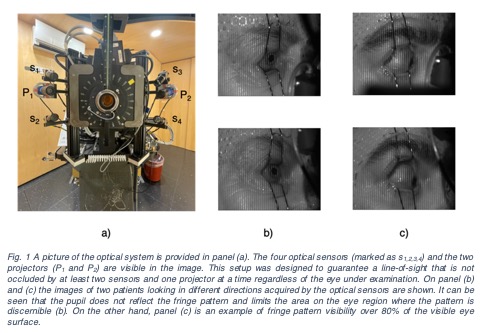
The optical system includes four cameras and two pattern projectors mounted on the nozzle (Fig. 1-a) allowing for pupil tracking via stereo-triangulation and three-dimensional fringe pattern profilometry of the visible surface of the eye. Fringe pattern analysis, based on the Fourier transform method, and ad-hoc calibration procedures were implemented to map the pattern deformation into physical coordinates that are consistent with the pupil localisation.
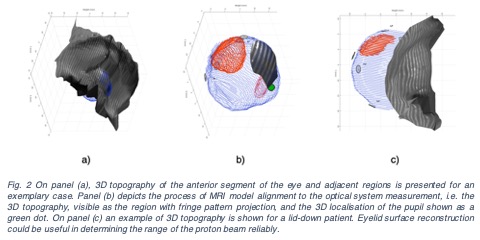
For comparing the optical-based tumour position estimates with X-ray measurements, the MR-based eye model is aligned to the clips position, through point-based registration, thus defining a reference tumour position according to the clinical standard. Afterwards, the corneal topography and pupil position (Fig. 2) were used in a constrained iterative closest point registration to obtain a corresponding clipless estimate of the eye position. The two measurements were compared to evaluate the performance of the optical system in measuring the tumour centre of mass position.
Results
Seventeen measurements of the eye position of three eye tumour patients acquired during the course of the treatment were included in the analysis. On average (standard deviation) the discrepancy in tumour position estimate was -0.21mm (1.10mm), 0.17mm (0.67mm), 0.29mm (0.84mm) and 1.33mm (0.79mm) in the X, Y, Z directions and in 3D, respectively. The data show that corneal topography of the entire visible ocular region is not always possible due to the absence of reflection of the projected pattern by the pupil (see Fig. 1). A moderate positive correlation between discrepancies and fringe pattern visibility within the eye was found (Pearson’s rho=0.51, p-value<0.05). Of note, when the fringe pattern was recognizable on more than 80% of the visible eye region, the mean discrepancy on 3D target localisation went down to 0.76 mm (0.20mm).
Conclusion
Sub-millimetric agreement in tumour position localisation was reported for the optical system compared to X-ray clips imaging, provided the projected fringe pattern was discernible in more than 80% of the region of interest (Fig. 1-b,c). In principle, an improvement of the reflection properties of the eye surface in the pupillary region could be achieved through the instillation of fluorescein. Corneal topography could prove useful not only to non-invasively verify treatment geometry but also to minimise range uncertainties, especially for patients treated through the eyelid (Fig. 2-c).