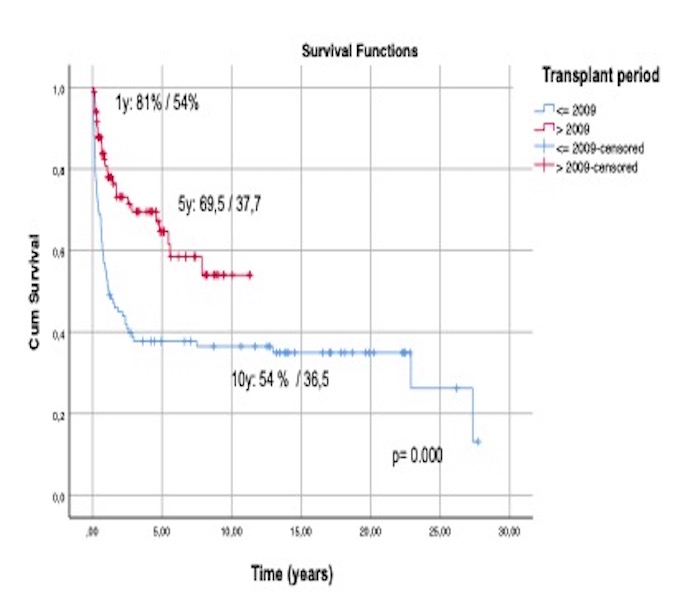
A total of 185 patients, 65 (35%) with ALL and 120 (65%) with AML were included. Median age was 38 years (18-59) and 83 were women (45%); 61% were in first complete remission. Median follow-up for survivors: 1,6 years (1-27). Nineteen patients had IPS (10,3%), and 7 of them died early after transplant. Most IPS cases were diagnosed before 2010 (15% vs 4,7%; p= 0,028) and all them received lung doses over 8.5 Gy. The 1y/5y-DSS were 61,4%/47,9% and 90,2%/81,4% before and after 2020, respectively (p=0,000) (Fig.1). Multivariate analyses showed that pre-transplant abnormalities in baseline chest X-Ray (p=0.001) and lung irradiation dose (p=0,005) were significantly associated with IPS development. In fact, the risk of pneumonitis increased four times for each Gy in the lungs. The 1y/5y-OS were 54%/37,7% before 2020 and 81%/69,5% after 2020 (p=0,000) (Fig2). Transplant period (before 2010), lung dose and development of pneumonitis were associated with lower OS (p=0,000).
Fig 1. Disease specific survival (death due to leukemia or related to the treatment were computed as events) (In red, patients treated since 2010 an in blue, patients treated before 2010)
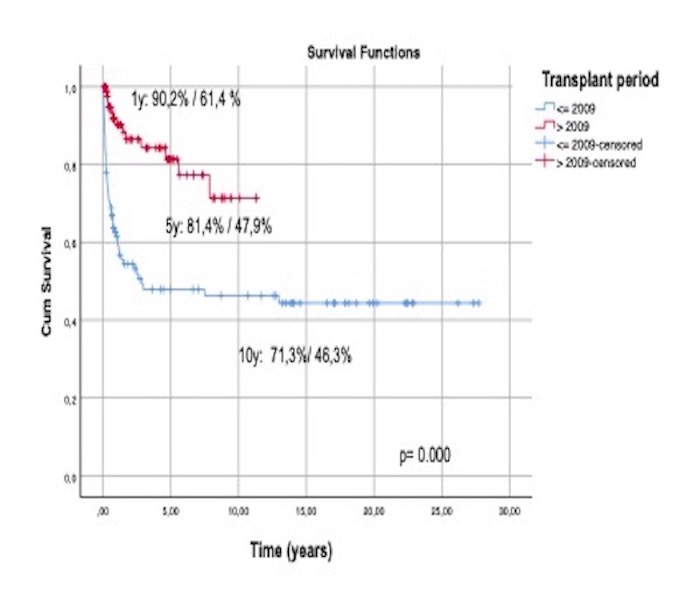
Fig 2. Overall survival (In red, patients treated since 2010 and in blue, patients treated before 2010)