Validation of intra-fraction adaptations for the MR-linac: novel drift correction and replanning
Madelon van den Dobbelsteen,
The Netherlands
OC-0279
Abstract
Validation of intra-fraction adaptations for the MR-linac: novel drift correction and replanning
Authors: Madelon van den Dobbelsteen1, Sara Hackett1, Hans de Boer1, Bram van Asselen1, Stijn Oolbekkink1, Bas Raaymakers1
1UMC Utrecht, Radiotherapy, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
A novel motion management functionality, enabling tumor tracking in real-time, will be available for the Unity MR-linac in 2023. If the tumor location shifts above a limit, the plan can be adapted using a baseline shift correction, called an intra-fraction drift correction. This development is promising for intra-fraction adaptations. The goal of this research is to show in silico dose outcomes of ten prostate patients for the novel intra-fraction drift correction compared to an existing clinically applied intra-fraction adaptation using in-house software, called intra-fraction replanning.
Material and Methods
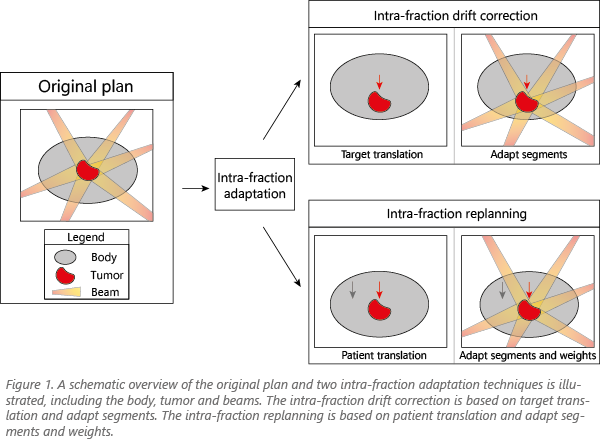
In our department an intra-fraction adaptation is performed for all prostate patients treated on the MR-linac, whereby a replanning adaptation occurs mid-treatment, enabling margin reduction. During delivery, a 3D MR-scan is acquired for replanning, using so-called adapt-to-position to translate all patient structures with adapt segments and weights. This process takes five minutes, and can be executed during delivery of the first half of the treatment. The intra-fraction drift correction developed by Elekta (Stockholm, SE) enables tumor tracking in real-time using two orthogonal 2D cine images and replanning if the tumor location shifts above a pre-defined limit. The plan is calculated without optimization based on 3D target translations only, the other structures remain in the original position. An overview of these methods is shown in Figure 1.
Monaco (v5.51.10) was used to analyze the dose of ten prostate patients, using drift correction and replanning, both mid-treatment. To compare five DVH metrics for both intra-fraction adaptations, the dose was recalculated on the same scan. The fractions of ten prostate patients, treated with intra-fraction replanning with a PTV margin of 2, 2, and 3 mm (LR SI and AP), were included. From 52 treated patients, these ten patients showed the lowest and highest translations in x, y, and z directions, to cover the full range of possible translations. The 3D translations ranged up to 6.2 mm.
Results
Figure 2 shows the DVH metrics of ten prostate patients. Significant differences were found for the PTV (p<0.01), rectum (p<0.01), bladder (p<0.01) and sphincter metrics (p=0.03), using a paired Student’s t-test. However, the dose differences are clinically irrelevant, and the OAR doses did not meet the criterion for only two fractions. Mean CTV values are similar for both intra-fraction adaptation techniques (p=0.36).
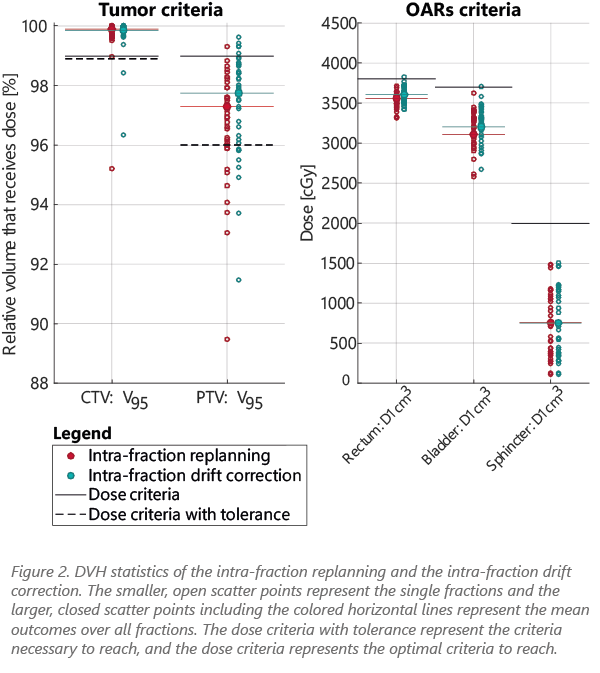
Conclusion
The in silico study showed good DVH outcomes for the intra-fraction drift correction and the intra-fraction replanning. The dose outcomes between the two intra-fraction methods are comparable, as the dose differences are clinically irrelevant. Intra-fraction drift corrections can be performed multiple times during a treatment, within one minute and with similar dose results compared to intra-fraction replanning. Therefore, this novel drift correction could be promising for intra-fraction adaptations for Unity MR-linac users.