Functional lung dose and postoperative lung complications in esophageal cancer trimodality therapy
Pieter Populaire,
Belgium
PD-0889
Abstract
Functional lung dose and postoperative lung complications in esophageal cancer trimodality therapy
Authors: Pieter Populaire1,2, Gilles Defraene3, Philippe Nafteux4,5, Lieven Depypere4,5, Karin Haustermans1,2
1Univeristy Hospitals Leuven, Department of Radiotherapy, Leuven, Belgium; 2KU Leuven, Laboratory of Experimental Radiotherapy, Leuven, Belgium; 3Laboratory of Experimental Radiotherapy, KU Leuven, Leuven, Belgium; 4Univeristy Hospitals Leuven, Department of Thoracic Surgery, Leuven, Belgium; 5KU Leuven, Department of chronic diseases and metabolism (CHROMETA), laboratory for respiratory diseases and thoracic surgery (BREATHE), Leuven, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
In trimodality therapy for esophageal cancer (EC), pulmonary postoperative complications (pPOCs) are related to the lung dose of neo-adjuvant chemoradiotherapy (nCRT). Meanwhile, studies in lung cancer have shown improved toxicity risk predictions when using dose metrics of the functional lung volume (FLV) instead of the anatomical lung volume. 4D-planning CTs can be used to identify the FLV leading to “functional avoidance planning strategies”. This exploratory analysis examines the role of FLV dose of nCRT for EC as a predictor of pPOCs.
Material and Methods
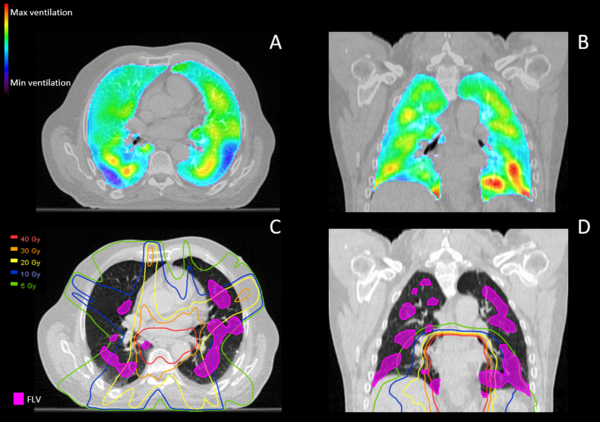
Patients treated in UZ Leuven between 01-2018 and 06-2022 with nCRT for EC using 4D CT-simulation were included in this analysis. Patients were treated to 45Gy in 25 fractions using IMRT, concomitant chemotherapy consisted of carboplatin-paclitaxel. Scans and treatment plans were imported and analysed in MIM Maestro. Total lung volume (TLV) was delineated on the maximum expiration phase. Jacobian determinants based on vector fields of the deformable image registration from maximum inspiration to maximum expiration respiratory phases were calculated (Figure 1 A+B). FLV was determined based on a 16% threshold of the maximum Jacobian determinant, analogous to the methodology described by Nyeng et al. (Acta Oncol. 2021) (Figure 1 C+D). Doses of the clinical treatment plan’s average image were non-rigidly registered to the maximum expiration phase (Figure 1 C+D). Volumes and derived absolute (mL) and relative (%) dosimetric parameters of the TLV and FLV (V40Gy, V30Gy, V20Gy, V10Gy, V5Gy, MLD) were extracted. Parameters were then compared between patients with and without pPOCs, using unpaired t-tests (normal distribution) or Mann-Whitney U-tests (non-normal distribution) using IBM SPSS.
Figure 1: Functional lung mapping
Results
Out of 51 patients, 12 patients with pPOCs were identified. Statistical analysis showed that the TLV was lower in the pPOCs group when compared to the non-pPOCs group (3141mL (SD: 858mL) vs 3601mL (SD: 635mL) p=0.025). The proportion of the TLV identified as functional (ratio FLV/TLV) was significantly higher in patients with pPOCs (29% (SD: 13%) vs 19% (SD: 11%) p=0.024). Finally, absolute (mL) FLV10Gy and FLV20Gy were significantly higher in patients with pPOCs (FLV10Gy: 360mL (SD: 216mL) vs 264mL (SD: 139mL) p=0.038; FLV20Gy: 166mL (SD: 106mL) vs 118mL (SD: 63mL) p=0.030). There were no statistical differences in relative nor absolute TLV10Gy (p= 0.326 and p=0.336) and TLV20Gy (p=0.159 and p=0.444) between both groups.
Conclusion
Our exploratory analysis shows that lower TLV is associated to the risk of developing pPOCs. Our findings also indicate that the absolute volume of high-functional lung that is exposed to a low to intermediate dose level (FLV10Gy and FLV20Gy) is prognostic of pPOCs. This can lead to improved toxicity prediction models and toxicity-limiting lung avoidance planning strategies for esophageal cancer.