Pattern of failure after SBRT for oligometastases: predictive factors for poli-progression
Davide Franceschini,
Italy
PD-0806
Abstract
Pattern of failure after SBRT for oligometastases: predictive factors for poli-progression
Authors: Davide Franceschini1, Veronica Vernier1,2, Luca Cozzi1,2, Luciana Di Cristina1,2, Antonio Marco Marzo1,3, Sara Stefanini4,2, Ciro Franzese1,5, Maria Massaro1, Marta Scorsetti1,2
1IRCCS Humanitas Research Hospital, Radiotherapy and Radiosurgery, Rozzano-Milan, Italy; 2Humanitas University, Biomedical Sciences, Pieve Emanuele-Milan, Italy; 3Humanitas University, Biomedical Sciences, Pieve Emanuele- Milan, Italy; 4IRCCS Humanitas Research Hospital, Radiotherapy and Radiosurgery, Rozzano-MIlan, Italy; 5Humanitas University, Biomedical Sciences, Pieve Emanuele, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients with oligometastatic disease (OMD), defined as a maximum of 5 metastases in utmost 3 different organs, can be safely treated with Stereotactic Body Radiation Therapy (SBRT). Despite most patients relapse with oligometastases, some of them can experience a poli-progression after a local ablative treatment (LAT). The purpose of this study was to retrospectively identify predictive factors of poli-progression in patients receiving SBRT for OMD.
Material and Methods
Data from a monocentric database were retrospectively analysed. Patients treated with SBRT for OMD and who developed progression after LAT were selected. Patients were categorized as oligo or poli-progressive according to the number of new/progressing metastases (< or > 5). Herein, we analyzed data about patients’ characteristics, oligometastatic presentation and radiation treatment characteristics to evaluate their relation with kind of progression. Univariate and multivariate Cox regression (backward conditional) model were used for this purpose.
Results
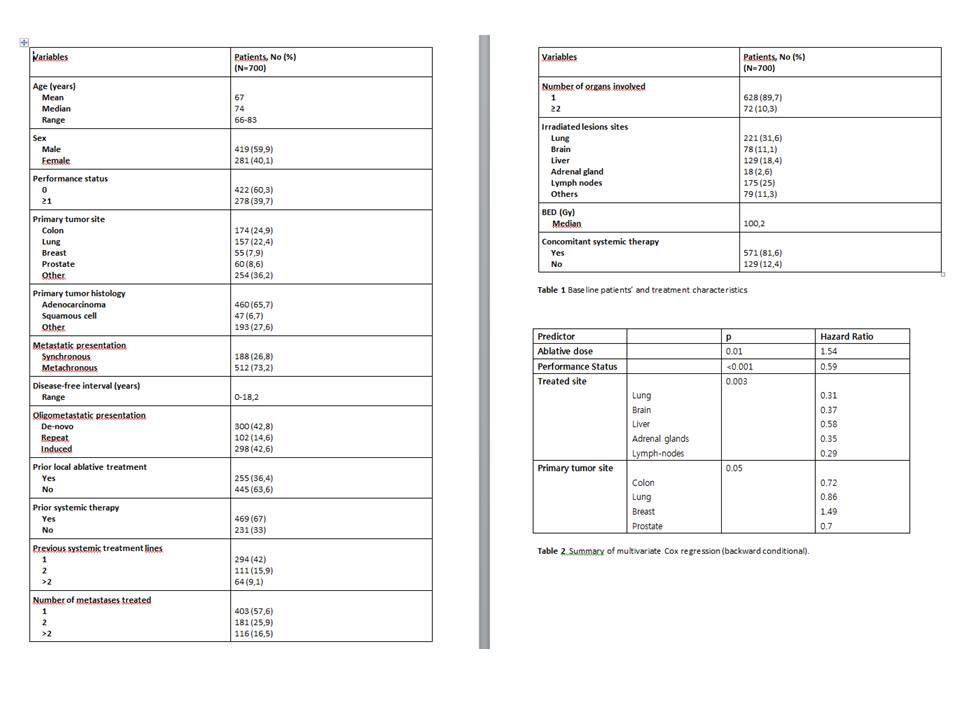
From 2013 to 2021, data from 1306 patients treated in our institution were collected. Of those, 700 progressing patients were retrospectively selected for this analysis. Baseline patients’ and treatment characteristics are summed in table 1.
During follow up 227 patients (32,4%) experienced a poli-progression; median time to poli-progression was 7.72 months (range 1-79.6).
Five variables predictive of poli-progression were found to be statistically significant at the univariate analysis: performance status (p<0.001), site of primary tumor (p=0.016), ablative dose (p = 0.002), treated site (p=0.002), single or double organ (p=0.03). Of those, four variables retained their significant predictive value on the multivariate analysis (table 2).
Conclusion
Our study identified four predictive factors associated with poli-progression in patients with OMD receiving SBRT. According to literature, OMD patients may have various clinical presentations, heterogeneity about the course of disease and outcomes. Our data may support comprehensive characterization of OMD, better understanding of factors associated with progression and eventually improve the management of specific subgroups of patients.