47/60 (78%) UK RT centres responded, with 36 (77%) complete responses. Centres have a median of 3 Clinical (Radiation) Oncology Consultants who treat TETs (range 0-12) and treat a median of 2-3 TETs per year (range: 0-1 [13%, 6/47] to 20+ [6%, 3/47]). Very few centres have a TET lead (19%, 9/47), a TET specialist nurse (6%, 3/47) or a TET specialist neurologist (23%, 11/47). Cases are generally discussed at local lung MDTs (64%, 30/47), but 85% (40/47) of respondents agreed TETs should be discussed at TET-specific MDTs due to their rarity.
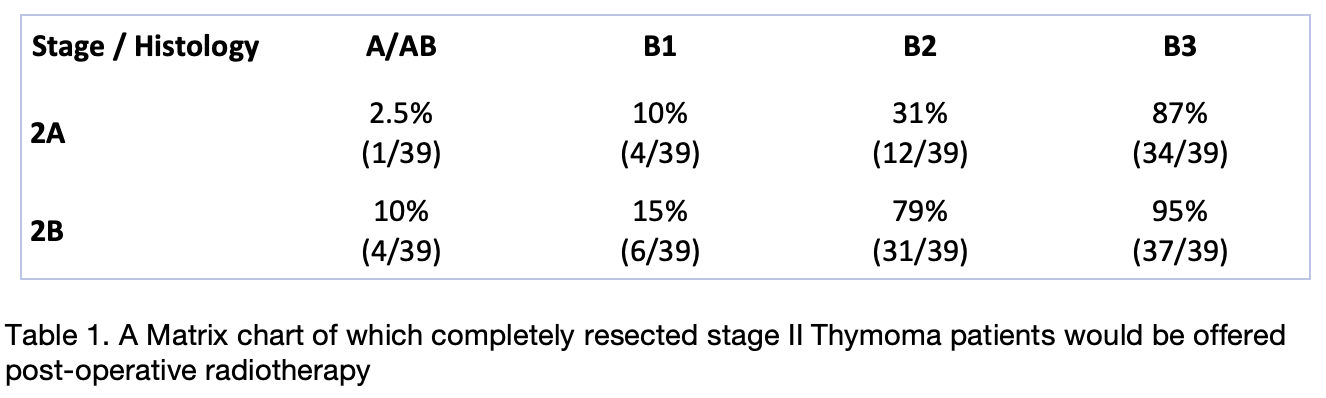
Most centres follow international guidelines when deciding to offer RT (91%, 43/47), of which the majority follow the 2015 ESMO guidelines (83%, 38/47). However, 23% would consider post-operative RT for some completely resected stage I Thymomas (9/39), and 23% would not offer post-operative RT for all stage III/IVa Thymomas (9/39). Additionally, as can be seen in Table 1, there is substantial variation in which patients with stage II Thymoma would be offered post-operative RT at different centre, with increasing stage and aggressive histology leading to increased concordance.
Regarding RT planning, 67% (24/36) use 4D-CT simulation, 86% (31/36) use VMAT, and 69% (25/36) use daily cone beam CT. A minority (17%, 6/36) include elective areas within their target volume, and 53% (19/36) vary their target volume based on resection status (19/19), histology (14/19) or stage (14/19). Peer review occurs with another Clinical (Radiation) Oncologist in 75% (27/36), with some centres utilising thoracic radiologists (11%) or thoracic surgeons (22%).
Follow up is primarily with Clinical (Radiation) Oncologists (89%, 32/36) and patients are generally seen six monthly (56%, 20/36) for five years (50%) or >7-10 years (31%). CT imaging is the most common imaging modality and occurs six monthly (36%) or annually (47%).