Online adaptive radiotherapy for low volume metastasized prostate cancer on the CyberKnife system
Victor Brand,
The Netherlands
PD-0741
Abstract
Online adaptive radiotherapy for low volume metastasized prostate cancer on the CyberKnife system
Authors: Victor Brand1, Maaike T.W. Milder1, Femke E.A.M. Froklage1, Miranda E.M.C. Christianen1, Kim C. de Vries1, Mischa S. Hoogeman1, Luca Incrocci1
1Erasmus MC Cancer Institute, University Medical Centre Rotterdam, Radiotherapy, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
The low α/β ratio of prostate cancer (PCa) suggests benefits of ultra-hypofractionation (UHF). However, for high-risk PCa patients this is challenging as seminal vesicles (SV) are included in the target volume. Our recently started UPRATE trial aims to prove the feasibility of SV PTV-margin reduction in low volume metastasized PCa patients. To this end, pre-treatment in-room CT-on-rails and online replanning are combined with intra-fraction fiducial tracking of the prostate on the CyberKnife. Here we present the plan protocol creation and validation in 10 patients, workflow optimization, and results of the first-in-men treatments.
Material and Methods
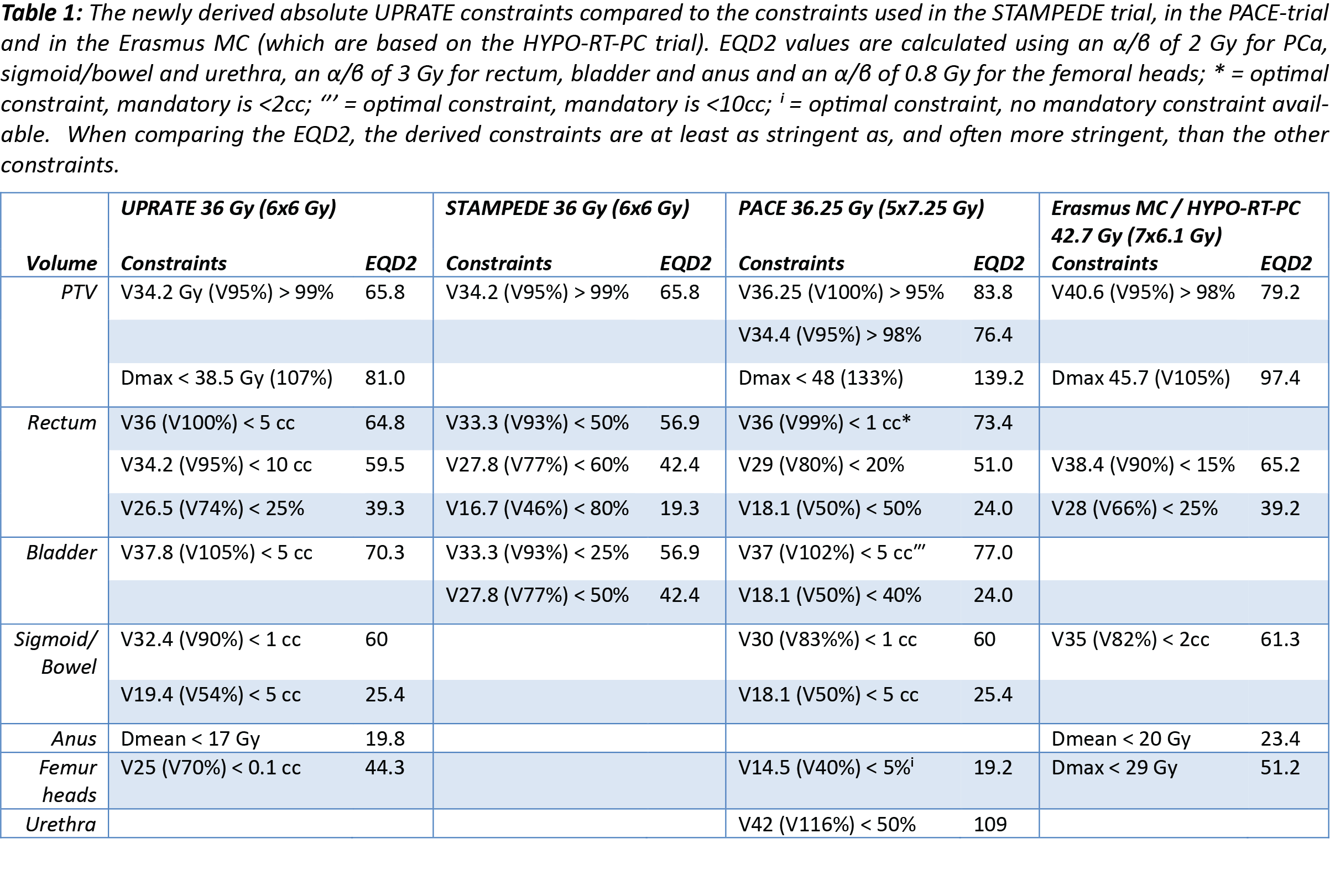
Patients are treated with 6 once-weekly fractions of 6 Gy according to the STAMPEDE trial on a CyberKnife with a CT-on-rails system. The organ-at-risk (OAR) constraints were derived from large randomized UHF trials, e.g. PACE and HYPO-RT-PC. To increase delineation and plan optimization speed during the online adaptation, volume constraints are turned into absolute constraints. Based on a planCT, a patient specific optimization script with reduced sample points (to reduce optimization time) was saved to run on the fraction CTs. This method was validated using 10 previously treated patients with 4 CTs each. For each fraction CT, the initial prostate contour is rigidly transferred on this new CT by aligning the implanted intraprostatic fiducials. The OARs and SV are segmented by artificial intelligence (AI). Rigid registration and AI was chosen after comparison with deformable image registration on adaptation time and inter-observer variation. A radiation oncologist adjusts these contours where needed. Treatment times of 2 end-to-end dummy runs were recorded.
Finally, the first four fractions delivered to our first UPRATE patient were timed and adherence to the constraints was recorded.
Results
Table 1 shows the UPRATE constraints compared to the STAMPEDE-, PACE- and HYPO-RT-PC-trial. These UPRATE constraints were met for 35/40 fractions for the 10 test patients. Of the 5 fractions that did not, 3 had bladder volumes <150 ml and 2 required PTV underdosage due to bowel within the PTV. The plan with reduced sample points, was clinically acceptable for 8/10 patients. Allowing individual template changes, a clinically acceptable fast optimization plan was achieved for all 10 patients. The end-to-end dummy runs took on average 55 minutes.
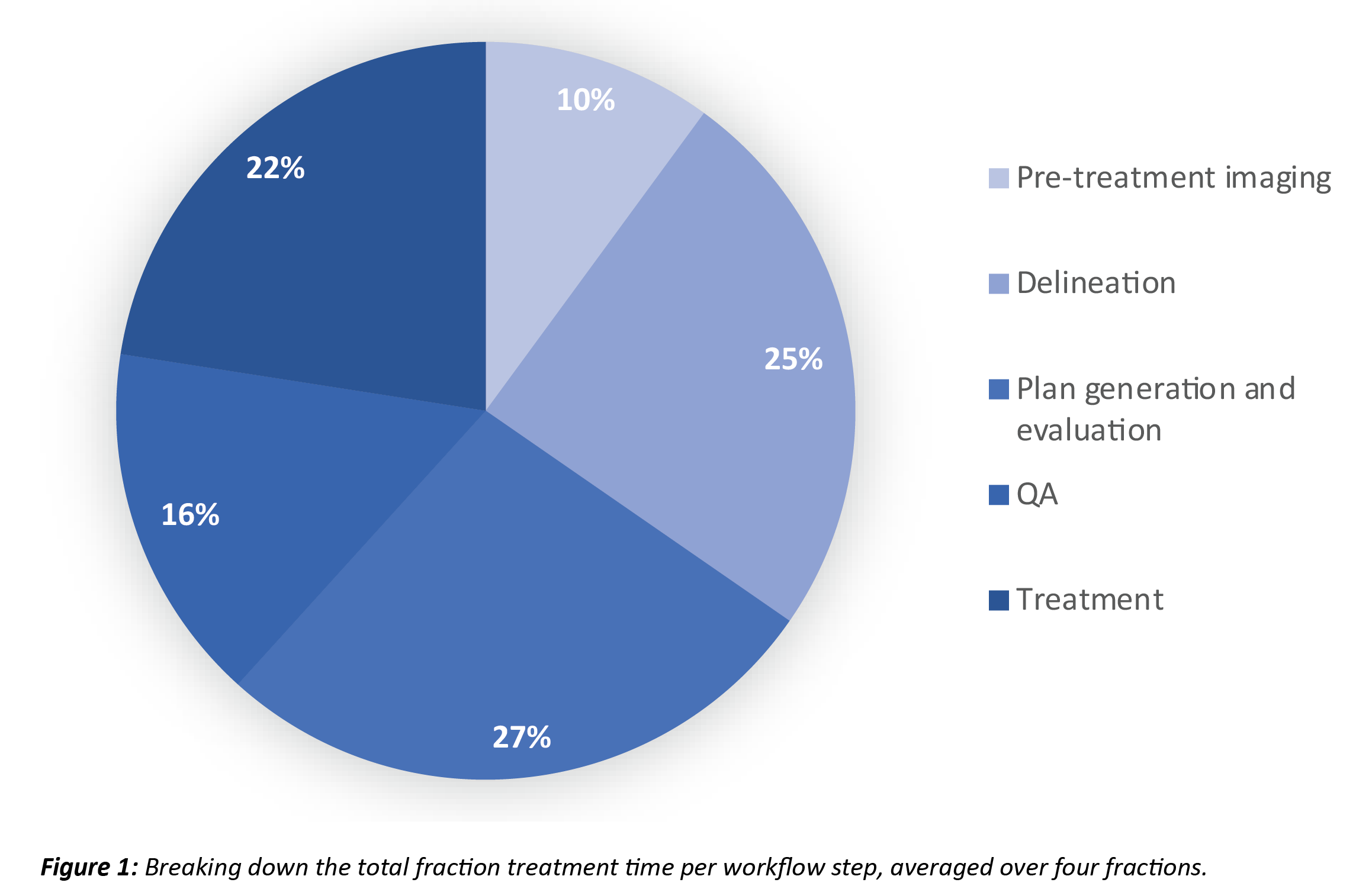
The average on-table time for the first four actually delivered fractions is 68 minutes. Figure 1 shows the percentage of time each individual workflow step accounted for. In only 1 delivered fraction a minor violation in PTV coverage (98.8%) was observed.
Conclusion
This study is the first step towards safely treating PCa patients with UHF when the whole SV needs to be treated and shows that online adaptive treatment on the CyberKnife is technically feasible, which was clinically demonstrated by the first patient treatment. We expect the total treatment time will reduce with ongoing experience in the UPRATE trial.