Ten-year outcomes of SBRT for oligometastatic breast cancer (OMBC): does synchronous OMBC benefit?
Sukhdeep Kaur Nagpal,
United Kingdom
PD-0240
Abstract
Ten-year outcomes of SBRT for oligometastatic breast cancer (OMBC): does synchronous OMBC benefit?
Authors: Sukhdeep Nagpal1, Komel Khabra2, Gillian Ross1, Anna Kirby1
1The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, Clinical Oncology, London, United Kingdom; 2The Royal Marsden NHS Foundation Trust, Research Data and Statistics Unit, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The benefits of SBRT in the management of metachronous oligometastatic breast cancer (OMBC) have been described in previous studies and its use in current clinical practice is established. However, the role of SBRT in the management of synchronous OMBC remains uncertain. Previous studies have shown superior survival outcomes for metachronous over synchronous oligometastatic disease, though a significant proportion of this evidence comes from the non-small cell lung cancer setting. SBRT for synchronous OMBC is not currently commissioned by the UK National Health Service but has been used in a private care setting. This retrospective review compares outcomes of SBRT-treated synchronous OMBC to those of SBRT-treated metachronous OMBC.
Material and Methods
We retrospectively analysed data of patients treated with SBRT for extra-cranial OMBC between December 2011 and April 2022. The study aimed to calculate progression-free survival (PFS), overall survival (OS), local control (LC), distant control (DC) and time to switch in systemic therapy (SACT). Survival analysis was performed using the Kaplan-Meier method with log-rank test. Toxicity was assessed using the CTCAE v5.0.
Results
A total of 74 OMBC patients with 113 lesions treated with SBRT were identified. Nine patients received SBRT again at a later date therefore, 85 separate episodes of SBRT were analysed. Median age at primary diagnosis was 48 years (range 23-72) with a median time from primary diagnosis to development of oligometastases of 42 months (range 0-292). The proportion of metachronous and synchronous oligometastases were 70% and 30% respectively. The most commonly prescribed dose/fractionation schedule was 30Gy in 3 fractions and the median biologically effective dose (BED at α/β = 10) was 60Gy (range 35.7-112.5Gy). In total 49% of patients switched SACT post-SBRT with a median time to switch of 14 months (range 0-79). Two patients (2%) experienced G3 acute toxicities (nausea/vomiting and diarrhoea). No ≥ G4 toxicities. Median follow up was 20 months (range 0-98). At 2 years the PFS was 39.0%, OS was 92.4%, LC was 85.9% and DC was 37.0% for the whole cohort. The 2-year LC rates were 86.5% and 85.8% and PFS rates were 35.3% and 48.3% for metachronous and synchronous disease respectively. The median PFS of metachronous and synchronous disease were 18 months (95% CI: 10.5 – 25.5) and 17 months (95% CI: 0.0– 36.8) respectively. Comparisons of LC and PFS for metachronous and synchronous disease were not statistically significant (p=0.87 and 0.86).
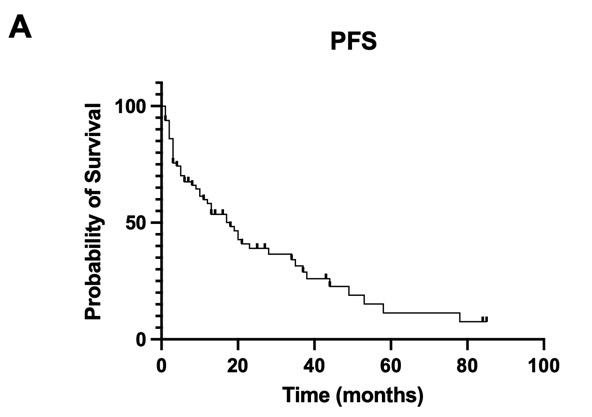
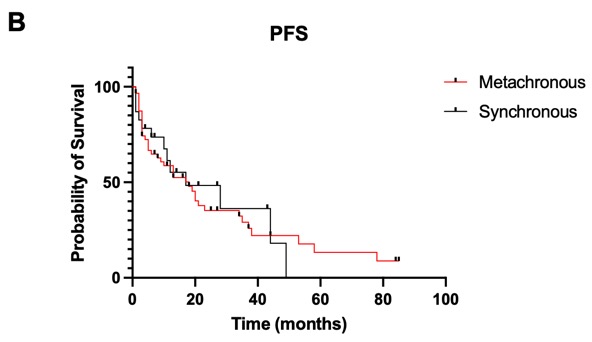
Figure 1: Kaplan-Meier curves of PFS for A) the entire cohort B) metachronous and synchronous OMBC
Conclusion
Our data confirms that SBRT is a highly effective, well tolerated treatment for OMBC with excellent LC rates regardless of metachronous or synchronous presentation. There is no suggestion that survival outcomes are inferior for synchronous disease. Further prospective studies are required to validate this comparison.