Dosimetric comparison: Virtual Unenhanced Dual Energy CT versus contrast CT for treatment planning
Maryam Afifah,
The Netherlands
PD-0661
Abstract
Dosimetric comparison: Virtual Unenhanced Dual Energy CT versus contrast CT for treatment planning
Authors: Maryam Afifah1, Duncan den Boer1, Loes Bulthuis1, Tezontl Rosario1, Jolanda Verbeek-Spijkerman1, Arjan Bel1, Zdenko van Kesteren1
1Amsterdam UMC, Radiotherapy, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
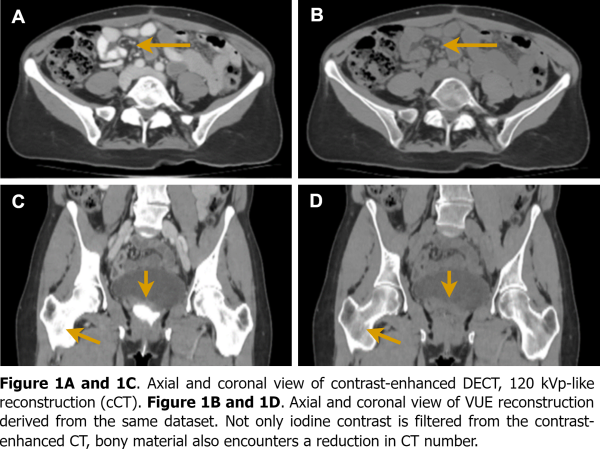
Purpose or Objective
Iodine contrast is commonly used to aid CT delineation in radiotherapy. However, this contrast is not present during treatment. A commonly employed strategy to account for this, is by applying a density override to the contrast-enhanced structures (CES) during treatment planning. Dual-Energy CT (DECT) is an emerging CT technique with the capability of generating virtual unenhanced (VUE) reconstructions from contrast-enhanced acquisitions, removing iodine-contrast from the images, eliminating the need to manually remove the CES. An observation from VUE images is that regions outside the CES, e.g. bones, also encounter a reduction in CT intensity, see Figure 1. The aim of this study is to assess the dosimetric effect of such a CT number reduction for treatment planning dose calculations based on VUE images, compared to the clinically used contrast-enhanced CT. The assessment is done in order to evaluate the feasibility of VUE application in the RT workflow.
Material and Methods
Scans of fifteen gynecological patients were included in this study. Iodine-based contrast agent was administered before acquiring a contrast-enhanced DECT scan (Revolution CT, GE Healthcare). Contrast consisted of intra-venous contrast, bowel contrast and vaginal contrast. Two reconstructions were made: one with 120 kVp-like reconstruction (cCT), generated from the two kilovolt peaks acquisition simulating a 120 kVp scan from conventional single-energy CT, and a VUE reconstruction. A clinical treatment plan (VMAT, 25 x 180cGy fractions resulting in 45Gy) was generated on the cCT with a density override (contrast agent to water) applied on the CES. Additionally, the dose distribution was calculated on the VUE reconstruction.
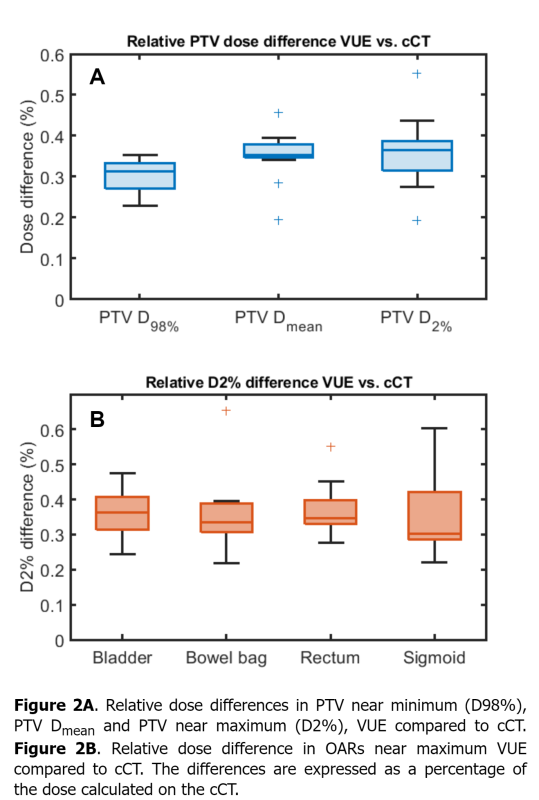
Comparison between dose distributions cCT and VUE, was done by evaluating the mean gamma values and pass rates (gamma analysis, 1%/1mm local dose with a dose cut-off of 30% of the global maximum dose). Furthermore, we reported differences in dose parameters of the PTV (D98%, Dmean and D2%) and near maximum doses (D2%) in the bladder, bowel bag, rectum and sigmoid.
Results
Suppression of the contrast agent by the VUE algorithm led to an average HU reduction of 186 (SD 75) HU in the CES compared to the cCT (average of 212 HU on cCT vs. 26 HU on VUE images).
The dose distributions calculated on the cCT and VUE images were close to identical. In fourteen subjects the gamma pass-rate was 100%, in one subject the pass-rate was 98%. The γmean was 0.16 (SD 0.03).
The PTV Dmean differed with a mean value of +16 cGy (0.35%) comparing VUE with cCT, see Figure 2A. The D98% and D2% differed with a mean value of +12 cGy (0.30%) and +17 cGy (0.36%), respectively. Figure 2B shows the differences in OARs near maximum doses, which were all well below 1%.
Conclusion
Differences between dose distributions calculated on the VUE reconstruction and the current clinical CT with density overrides are minimal (below 0.5%). This demonstrates the feasibility of VUE application in the RT workflow regarding treatment planning.