Daily Bolus Position Variability with Dosimetric Implications in Adjuvant Breast Cancer Radiotherapy
Ghizela Ana Maria Salagean,
Romania
PO-2306
Abstract
Daily Bolus Position Variability with Dosimetric Implications in Adjuvant Breast Cancer Radiotherapy
Authors: Ghizela Ana Maria Salagean1,2, Krisztina Varga1, Laszlo Kun-Balint1, Daniela Cojocaru1, Radu-Vlad Neag1, Mihai Cojocaru-Laboncz1, Andreea-Florentina Cudlici1, Cozmin Duran1, Zoltan Balint2, Daniel Portik1
1TopMed Medical Centre, Radiotherapy, Targu-Mures, Romania; 2Babes Bolyai University, Faculty of Physics, Cluj-Napoca, Romania
Show Affiliations
Hide Affiliations
Purpose or Objective
Bolus material is a tissue equivalent material commonly used on the skin surface of the patient to maximize or add radiation dose to an irradiated area during radiotherapy (RT). In this study we analyzed the position variability of the bolus material and the dosimetric changes it determines in target volume (TV) coverage and the organ at risk (OAR)
Material and Methods
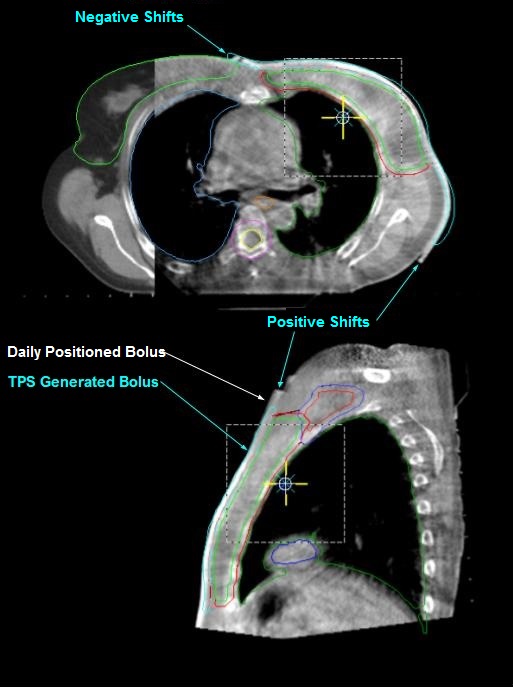
We retrospectively evaluated 8 cases of breast cancer irradiation in which bolus materials were used to obtain better skin surface coverage. Adjuvant RT was administered at a dose of 50Gy in 25 fractions, to the chest wall ± nodal regions. For each patient, the daily positioning variability was noted, and the movement of the bolus was categorized as being either a ‘positive’ shift (PosS) or a ‘negative’ shift (NegS) (Figure 1).
Afterwards, a second dosimetric plan was created in which the coordinates of the average bolus positioning variation were used. Finally, we made a retrospective comparison between the initial and recalculated dosimetric plans.
Results
The coverage of TV was respected (D95%>95%). However, in some cases we could notice a modification of the hotspots’ position and values going over the 107% threshold (Table 1).
| Treated plan |
|
| Recalculated plan PosS |
|
| Recalculated plan NegS |
|
|
| Dmax (%) | Dmax position | PTV N* 95% | Dmax (%)
| Dmax position
| PTV N 95%
| Dmax (%)
| Dmax position
| PTV N 95%
|
| P1 | 105.5 | PTV N | 98.0 | 105.7 | PTV IMN**
| 95.6 | 105.4 | PTV IMN
| 97.8 |
| P2 | 107.1 | PTV N
| 98.8 |
|
|
| 109.6 | PTV
| 98.5 |
| P3 | 107.1 | PTV*** | 97.2 | 108.1 | PTV | 98.1 | 107.9 | PTV | 97.1 |
| P4 | 104.6 | PTV IMN | 97.8 | 104.6 | PTV IMN
| 98.3 | 104.6 | PTV
| 97.9 |
| P5 | 105.7 | PTV | 99.6 | 106.5 | PTV N
| 99.6 | 105.9 | PTV N
| 99.5 |
| P6 | 106.6 | PTV IMN | 99.0 | 106.6 | PTV IMN | 99.4 | 107.2 | PTV IMN | 99.4 |
| P7 | 105.2 | PTV N | 97.7 | 104.6 | PTV N | 97.5 | 104.9 | PTV N | 98.0 |
| P8 | 106.8 | PTV IMN
| 96.0 | 106.4 | OUT of PTV | 97.2 |
|
|
|
*PTV N-PTV Axilla, **PTV IMN- PTV Internal Mammary Nodes, ***PTV-PTV Chest Wall
While we could not observe significant statistical differences, when we evaluate the dose for OAR, we could highlight some individual cases where the differences could raise some concerns. For mean heart dose, we obtained an average of 4.1±0.3Gy, as compared to 3.5±0.4Gy for PosS and 4.1±0.6Gy in the case of NegS. The lung V5, V20 and Dmean were 40.9±17.9%, 21.2±9.7% and 11.1±4.3Gy, as compared to 47.0±11.2%, 24.9±7.3% and 12.7±3.2Gy in PosS cases and 38.4±18.9%, 19.6±10.3% and 10.4±3.8Gy for NegS, respectively. The TV coverage was affected in PTV N, when the bolus shift in craniocaudal direction was significant, from a 98.0±1.5% it decreased to 96.6±1.6% with PoS and it increased to 98.3±1.2% with NegS.
Conclusion
In this small retrospective study, we determined that the daily position variability of the bolus material does not significantly modify the distribution of the delivered dose to the TVs or OAR. However, we observed that hotspots may suffer alterations, especially concerning the axillary region. A larger, multicentric study is warranted to evaluate these effects on the daily practices of RT departments.