A predictive model to determine optimal breath-hold parameters in breast radiotherapy
PO-2271
Abstract
A predictive model to determine optimal breath-hold parameters in breast radiotherapy
Authors: Domenico Piro1, Francesca Gruosso1, Michele Aquilano1, Althea Boschetti1, Francesco Catucci1, Andrea D'Aviero1, Paolo Gaias1, Martina Iezzi1, Marco Marras1, Sebastiano Menna1, Danila Piccari1, Elisa Pilloni1, Francesco Preziosi1, Flaviovincenzo Quaranta1, Alessia Re1, Nadia Ulgheri1, Valeria Verusio2, Claudio Votta1, Vincenzo Valentini3, Davide Cusumano1, Gian Carlo Mattiucci1
1Mater Olbia Hospital, Radiotherapy, Olbia (SS), Italy; 2Università Cattolica del Sacro Cuore, Istituto di Radiologia, Roma, Italy; 3Fondazione Policlinico Universitario A. Gemelli IRCCS, Dipartimento di Diagnostica per Immagini, Radioterapia Oncologica ed Ematologia, Roma, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The breast radiotherapy treatment is today usually administered in breath hold condition, especially for the left side, to reduce the dose received by the heart.
In our Institution a spirometer-based system able to monitor the lungs volume is used to manage the intrafraction motion. During the simulation procedure, a respiratory band is set with a bandwidth arbitrary defined by the radiation therapist (RTT).
The aim of this study is to propose a predictive model able to calculate the probability of obtain suboptimal fractions starting from the defined bandwidth.
Material and Methods
For this study 58 breast cancer patients (50 left; 8 right) treated in breath-hold were enrolled.
During CT simulation, each patient received a coaching session where three breath-holds of 25 seconds were acquired. Based on these breaths, the maximum breathing capacity was determined, and the breath-hold level was placed at 85% of the maximal breath-hold level.
The breath-hold bandwidth was arbitrary chosen by the RTT managing the CT simulation.
Daily CBCT was acquired each day of treatment, asking the patient to reproduce the breath hold level established during CT simulation.
The body difference between simulation CT and CBCT image was measured, with the aim of quantifying inter-fraction variability present in each RT fraction after the couch shifts compensation.
The absolute difference in terms of body between the first daily CBCT and planning CT was calculated along each beam axis. A treatment fraction was defined as “non-optimal” when the difference between CT image and CBCT was at least 4 millimetres in one of the beam axes.
The ability of the bandwidth of predicting the probability of occurring a not-optimal fraction during treatment was investigated using the Wilcoxon Mann–Whitney test, setting a value of p<0.05 as significance level. A linear regression model was then calculated, and the predictive performance was evaluated in terms of area under Receiver Operating Characteristics (ROC) curve (AUC).
Results
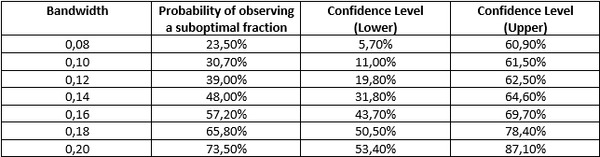
A total of 24 patients out of 58 observed showed a variation greater than 4 millimetres at the first treatment fraction. This variation is significantly correlated with the bandwidth (p=0.034), resulting in a predictive model with an AUC of 0.65. The probability of observing a ‘not optimal fraction’ in function of the bandwidth are reported in table 1.
Conclusion
Using data reported in table 1, it is possible to provide the RTT with a tool to minimize the risk of an adverse event during treatment, considering patient compliance and prescription dose.