Bladder filling verification with bladder scan for prostate radiotherapy: how reproducible we are?
Davide Giovanni Bosetti,
Switzerland
PO-2269
Abstract
Bladder filling verification with bladder scan for prostate radiotherapy: how reproducible we are?
Authors: Davide Giovanni Bosetti1, Gianfranco Angelo Pesce1, Stefano Leva1, Francesco Mosè Castronovo1, Thomas Zilli1, Matteo Coppotelli2, Stefano Presilla2, Maria Antonietta Piliero2
1Ente Ospedaliero Cantonale EOC, Radiation Oncology Clinic, Bellinzona, Switzerland; 2Ente Ospedaliero Cantonale EOC, Medical Physics Division, Bellinzona, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
About 5-10% of men undergoing curative radiotherapy for prostate cancer develop radiation cystitis. Adequate bladder filling at simulation and during treatments can reduce bladder irradiation and the consequent risk to develop treatment-related side effects. Bladder scanners can be easily implemented in the treatment workflow to ensure correct bladder filling and treatment reproducibility. Aim of the present study is to assess the accuracy in bladder volume measurements of a commercial available bladder scan.
Material and Methods
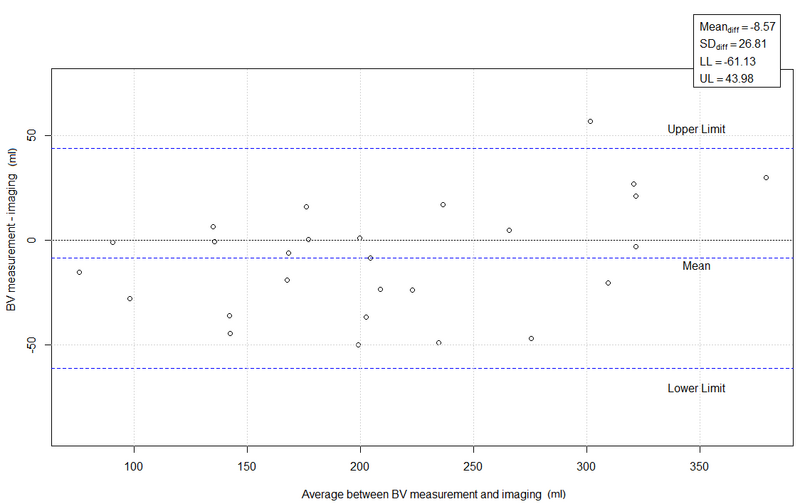
Data of sixteen consecutive patients with prostate cancer undergoing definitive (13 = 81.3%) or salvage (3 = 18.7%) radiotherapy were analyzed. All men were treated with Volumetric Modulated Arc Therapy with a total dose of 78Gy and 64-66Gy in 2-Gy per fraction for primary and salvage treatments, respectively. Bladder scan measurements were performed immediately prior to the CT simulation or the pre-treatment CBCT scan. The bladder structure was contoured on the acquired images by a radiation oncologist. Bladder volumes estimated with the bladder scan were compared with volumes measured using the planning CT or CBCT scans. Twenty-seven pairs of data were collected and analyzed. Bland-Altman plot and Lin’s correlation concordance coefficient were used to evaluate the accuracy and precision of the bladder scan i10®. The results were compared with the contouring inter-operator variability. The bladder was contoured on 16 images by a radiation oncologist, a medical dosimetrist and a radiotherapy technologist. For each image, the standard deviation of the bladder volumes was calculated. Inter-operator variability was estimated as the mean value of the standard deviations.
Results
The image-based bladder volumes ranged from 83 to 364 ml. The Bland-Altman plot (figure a) showed a mean difference of -8.6 ml (range: -61.1 - 44.0 ml) in bladder volumes measured with the two modalities. These differences were independent from the bladder volume. The results were confirmed by the Lin’s concordance correlation coefficient that showed bias correction factor Cb= 0.99 (high accuracy) and Pearson correlation coefficient ρ=0.95 (moderate precision). The inter-operator variability was 10.7 ml (1 standard deviation), while the precision of the bladder scan was 26.8 ml (1 standard deviation). The larger range of variability of the measurements could be due to the bladder wall volume that is included in the images but not in the scanner measurements.
Conclusion
Assessment of bladder filling using a bladder scan acquired before planning CT simulation or radiotherapy treatments showed a high rate of reproducibility. Routine implementation of this technology in the clinical practice is expected to improve the reproducibility of daily treatments, reduce daily imaging burden, and improve patient’s compliance.