Patient position verification for multi isocenter total body irradiation with VMAT
Annelies Zoetelief,
The Netherlands
PO-2265
Abstract
Patient position verification for multi isocenter total body irradiation with VMAT
Authors: Annelies Zoetelief1, Tessa Harderwijk1, Bianca Hoeben1, Mirjam Willemsen-Bosman1, Lean Krikke1, Enrica Seravalli1
1University Medical Center Utrecht, Radiation Oncology, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
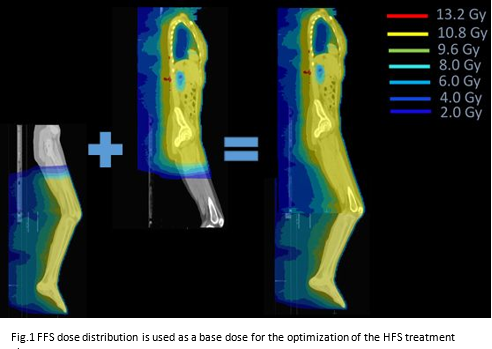
In August 2021, we implemented multi isocenter Volumetric Modulated Arc Therapy (VMAT) Total Body Irradiation (TBI) in combination with a rotatable tabletop at our department. The dose optimization and treatment are performed consecutively in Head First Supine (HFS) and in Feet First Supine (FFS) orientations. The patient Position Verification (PV) procedure is performed for the HFS and FFS treatment plans separately on different parts of the patient's anatomy, using cone beam computed tomography (CBCT). PV online corrections could potentially lead to over- or underdosage in the overlap zone (Fig.1). The aim of this retrospective study was to evaluate the necessity of longitudinal online correction of the FFS plan.
Material and Methods
The tabletop (IT-V medizintechnik, Austria) allows rotation from HFS to FFS orientation, while the patient remains immobilized in an individualized whole body vacuum mattress and open face mask. The treatment plan is optimized on the HFS and FFS Computer Tomography (CT)-scans, co-registered on the overlapping anatomical region (Fig.1). Depending on patient-length, 4 to 7 isocenters with overlapping arcs are applied. Prescription dose is 12 Gy in 6 (twice-daily) fractions with mean dose constraint for lungs <8 Gy, kidneys <10 Gy and lenses <6 Gy, conform ESTRO recommendation. The distance between the isocenters is automatically applied to the treatment table from the control room using Theraview (Cablon Medical, Netherlands) software.
Setup data of 11 patients (height range: 111-200 cm), 62 fractions, was analyzed.
The intended longitudinal distance between the HFS and FFS isocenters was per treatment compared to the calculated distance between the isocenters with and without online FFS patient position correction. The longitudinal distance between HFS and FFS isocenters was calculated by using the absolute treatment table values.
Results
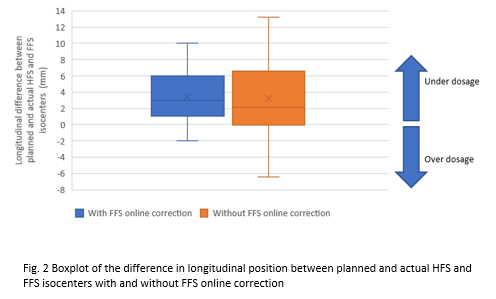
The average absolute difference (± stdev) in longitudinal position between planned and per treatment calculated HFS and FFS isocenters was 4 ± 3 mm and 5 ± 4 mm with and without FFS online correction, respectively. On average, the FFS and HFS dose distributions moved 3 mm apart, both with and without FFS online correction (Fig. 2).
Conclusion
By applying an FFS online correction, the average absolute difference in the longitudinal direction between planned and per treatment HFS and FFS isocenters is reduced by 1 mm, and the range becomes smaller than when the FFS online correction is not applied. However, because of this small analyzed difference, the FFS CBCT can be omitted, which shortens the overall treatment time. This reduces the chance of intrafraction patient movement and increases patient comfort. Because of outliers, attention should still be paid to the robustness of the dose distribution in the HFS and FFS overlapping region.