Assessment of weight loss and setup reproducibility in nasopharyngeal cancer patients.
PO-2264
Abstract
Assessment of weight loss and setup reproducibility in nasopharyngeal cancer patients.
Authors: Kok Ming Lee1, Shi Ying Goh2, Nianci Liu1, Sze Yarn Sin1, Heather Jia Hui Tan1, Emily Caluraud1, Semaya Natalia Chen1, Sharon Mei Mei Wong1, Eric Pei Ping Pang1
1National Cancer Centre Singapore, Division of Radiation Oncology, Singapore, Singapore; 2Singapore Institute of Technology , Faculty of Health and Social Science, Singapore, Singapore
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy with or without concurrent chemotherapy (CCRT) are the primary treatment modality for nasopharyngeal carcinoma (NPC). Accurate positioning and reproducibility are paramount in radiotherapy for NPC patients, due to its fairly large treatment field extending from nasopharynx to the neck region. Image matching at high dose region near the clivus are commonly prioritized over the neck nodal region due to its proximity to critical organs-at-risks (OARs). This study aims to assess the impact of weight loss on the deviation of lymph node planning target volume (LN-PTV) from the primary planning target volume (P-PTV) and the effectiveness of existing guidelines for repeated CT (re-CT).
Material and Methods
This retrospective study recruited 44 locally advanced NPC patients with nodal involvements from October 2019 till December 2020. Among these patients, 16 had repeated CT scans midway through due to weight loss and contour changes. A total of 253 weekly cone-beam computed tomography (CBCT) images were reviewed offline. To determine the degree of setup errors without re-setup interventions, only the initial pre-corrected CBCT of the weekly treatment session was used for data analysis. Differences in the setup errors between the P-PTV and LN-PTV were assessed in six-degree of freedom; superior-inferior (SI), left-right (LR), anterior-posterior (AP), yaw (Y), pitch (P) and roll (R). Weight loss between the groups (without and with re-CT) were compared.
Results
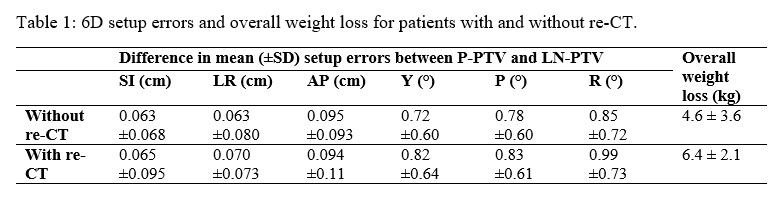
Minimal difference in the mean setup errors were observed between the P-PTV and LN-PTV for patients with or without re-CT in the translational (<1mm) and rotational (<1⁰) planes (Table 1). There was a statistical difference in weight loss between patients without re-CT (4.6 ± 3.6kg, 6.6%) compared to those with re-CT (6.4 ± 2.1kg, 9.4%) (p<0.001).
Conclusion
Existing guidelines and selection of patients for re-CT has demonstrated effectiveness in maintaining setup reproducibility with acceptable alignment of P-PTV and LN-PTV observed. Patients who underwent re-CT exhibited a greater percentage of overall weight loss compared to those without re-CT.