An evaluation of IGRT strategies in N1 prostate cancer patients receiving nodal irradiation
Danielle Fairweather,
United Kingdom
PO-2257
Abstract
An evaluation of IGRT strategies in N1 prostate cancer patients receiving nodal irradiation
Authors: Danielle Fairweather1, William Kinnaird1, Helen Grimes2, Reena Davda3, Lauren Taylor1, Amanda Webster1
1University College London Hospital, Radiotherapy and Proton Beam Therapy, London, United Kingdom; 2University College London Hospital, Medical Physics, London, United Kingdom; 3University College London Hospital, Department of Uro-oncology, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The benefits of pelvic ± para-aortic nodal (PAN) irradiation in N1 prostate cancer patients are currently being debated. However, data regarding the optimal IGRT strategy for these patients is limited. This evaluation aims to quantify the inter-fraction motion of pelvic and para-aortic lymph nodes targets in this patient cohort. This will help to establish if our current protocol of daily extended field of view (EVOF) volumetric imaging is required in the PAN region.
Material and Methods
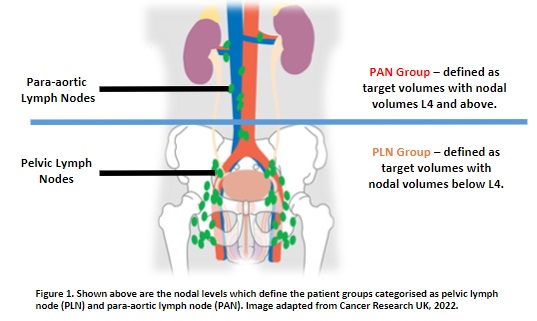
Approval was given by the departmental governance group. 23 patients with N1 prostate cancer who received daily online IGRT from May 2021–October 2022 were selected. Patients were categorised as pelvic LN (PLN) or PAN, Figure 1. All CBCTs were retrospectively visually assessed and registered to the planning CT using 3 registration methods: intensity range - bones, structure VOI - pCTV, and structure VOI - nCTV. All CBCTs that required patient reset up were excluded. Data was stored on a secure computer. Inter-fraction motion was evaluated in excel by calculating independent prostate motion, LN motion, and total LN displacement from prostate. The mean, systematic (Σ) and random error (σ) was calculated.
Results
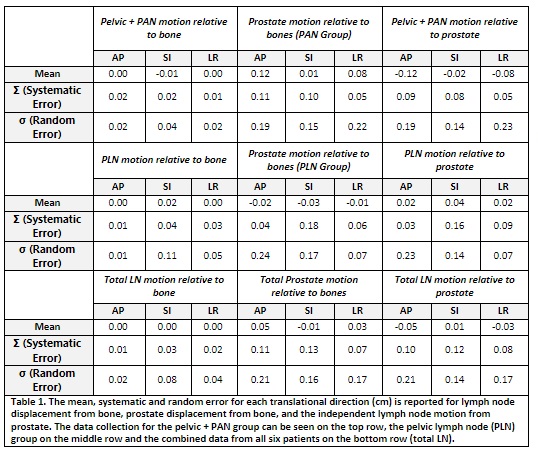
6 patients to date are reported from this evaluation. 117 CBCTs were retrospectively reviewed, and 351 image registrations were undertaken. 3 patients received irradiation to the PAN, and 3 received irradiation to the PLN. In total, 4 patients required EVOF stitched-CBCTs to visualise the full length of PTVs (3 PAN, 1 PLN). The mean (± Σ) nodal displacement from bones in the PAN group in the AP, SI and RL direction was 0.00(0.02), -0.01(0.02) and 0.00(0.01)cm, respectively. In the PLN group, the mean (± Σ) nodal displacement from bone in the AP, SI and RL direction was 0.0(0.01), 0.02(0.01) and 0.0(0.03)cm. The mean (± Σ) nodal displacement from prostate in the PAN group in the AP, SI and RL were 0.02(0.03), 0.04(0.16) and 0.02(0.09)cm, respectively. The mean (± Σ) nodal displacement from prostate in the PLN group were -0.12(0.09), -0.02(0.08) and -0.08(0.05)cm in the AP, SI and RL direction. The σ for all displacements are reported in Table 1.
Conclusion
Initial data review suggests there is limited independent displacement between LN relative to bony anatomy. This implies that bony anatomy could be used as a match surrogate for N1 prostate patients receiving nodal irradiation. As a result of this, the current IGRT protocol for these patients is under review, with a view to remove daily EFOV-CBCT. An EFOV-CBCT would instead be done on a weekly basis, with a CBCT at prostate/PLN level followed by a kV/kV pair at the level of superior nodal disease being done daily. The aim of this evaluation was to ensure that N1 prostate patients are receiving safe IGRT with concomitant doses that are ALARP. The new proposed protocol would decrease the imaging dose as well as treatment time. Data analysis will continue for the remaining 17 patients and if findings align, a new IGRT protocol will be implemented.