Is photo biomodulation effective in managing oral mucositis in head and neck radiotherapy?
Elaine Smith,
United Kingdom
PO-2249
Abstract
Is photo biomodulation effective in managing oral mucositis in head and neck radiotherapy?
Authors: Elaine Smith1, Vicky Poole2, Eloise Casey3
1Gloucestershire Hospitals NHS Foundation Trust, Gloucestershire Oncology Centre, Cheltenham, United Kingdom; 2Gloucestershire Hospitals NHS Foundation Trust, Oncology, Cheltenham, United Kingdom; 3Gloucestershire NHS Foundation Trust, Radiotherapy, Cheltenham, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients undergoing radiotherapy or chemoradiotherapy for head and neck malignancies suffer from complications such as oral mucositis (OM); dysphagia; pain; xerostomia and dysgeusia. These toxicities can be treatment dose limiting; may require further medical interventions or even admission and have a serious effect on patients’ quality of life. A recent systematic review of the literature recommended the use of photo biomodulation (PBM) intra-orally for patients receiving radiotherapy +/- chemotherapy for head and neck cancer to manage OM.
This study is one departments perspective on using PBM in managing OM during radiotherapy for head and neck malignancies.
Material and Methods
Between May 2022 and October 2022 24 patients receiving radiotherapy for head and neck malignancies were approached regarding the use of PBM, 20 patients proceeded. Patients used the PBM unit before or after each fraction of radiotherapy. Patients were reviewed weekly by the head and neck clinical nurse specialist and a record of their OM score was recorded according to the World Health Organisations OM scoring system. Patients were also asked to self- score their OM on a weekly survey which also asked for comments regarding the use of PBM. Thematic analysis of patient’s comments gave qualitative data on the use of PBM. A retrospective control group of 20 patients with similar diagnosis and radiotherapy treatment regime was used as a comparison. This group of patients followed the departments current OM treatment pathway.
Results
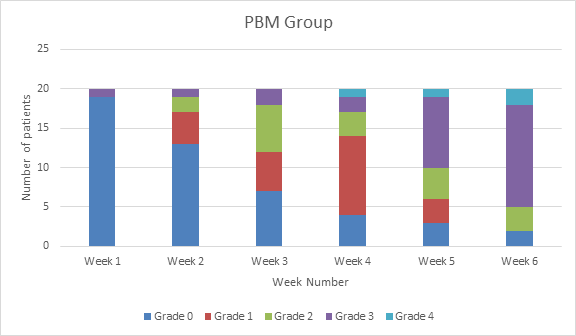
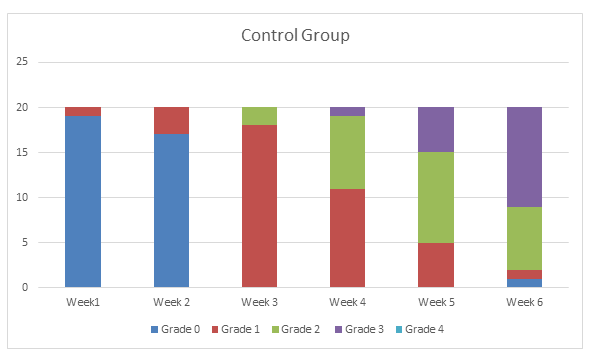
The results show that, ignoring the patient with grade 3 OM from the start of treatment, 2 patients had grade 2 OM in week 2, one week earlier than in the control group. Grade 2 OM is classed as significant in this project as it is the point where patients require further intervention. In the PBM group 35 % of patients required Caphosol, 60% required Gelclair. In the control group 50% of patients required Gelclair but this is the departmental pathway for treatment of OM.
Both the PBM and control group results are very similar. In the final week of treatment both the PBM group and the control group had the same number, 90%, of patients with significant OM. The major difference was two patients had grade 4 OM in the PBM group and this level of OM was not seen in the control group.
Themes identified from the patient’s comments were
1 Ease of use
2 Uncertainty of benefits
3 Size of applicator- painful when radiotherapy side effects start
Conclusion
The overall aim was to evaluate the use of PBM in the effective management of OM in patients receiving radiotherapy. In the acute setting PBM has not shown to be significantly more effective than the department’s current pathway for the management of OM, however PBM may hold some benefit in the management of other radiotherapy side effects.