Dosimetric results of a randomised trial of HDR vs. LDR single dose BT of localised prostate cancer
PO-2196
Abstract
Dosimetric results of a randomised trial of HDR vs. LDR single dose BT of localised prostate cancer
Authors: Georgina Fröhlich1, Péter Ágoston1, Kliton Jorgo1, Tibor Major1, Zoltán Takácsi-Nagy1, Csaba Polgár1
1National Institute of Oncology, Centre of Radiotherapy, Budapest, Hungary
Show Affiliations
Hide Affiliations
Purpose or Objective
To present dosimetric comparison of single fraction interstitial high-dose-rate (HDR) and low-dose-rate (LDR) brachytherapy (BT) in localised prostate cancer.
Material and Methods
The PROMOBRA prospective randomised clinical trial (ClinicalTrials.gov: TC02258087) was initiated at our institution to compare the clinical results of HDR vs. LDR BT as monotherapy of organ-confined prostate cancer. Between 2015 and 2022, 250 patients were randomly assigned to receive either HDR BT (123 pts) with one fraction of 19 (48 pts) or 21 Gy (74 pts) or permanent LDR I-125 seed BT with 145 Gy (127 pts). HIPO inverse optimization algorithm was used for HDR and IPSA for LDR planning. Final dosimetry of HDR treatments was based on updated needle and contour positions in transrectal ultrasound. Stranded seeds with mean activity of 0.56 mCi (0.50-0.60 mCi) were implanted after preimplant treatment planning using intraoperative (live) planning, and the postimplant planning was based on CT-MRI image registration 4 weeks later (Figure).
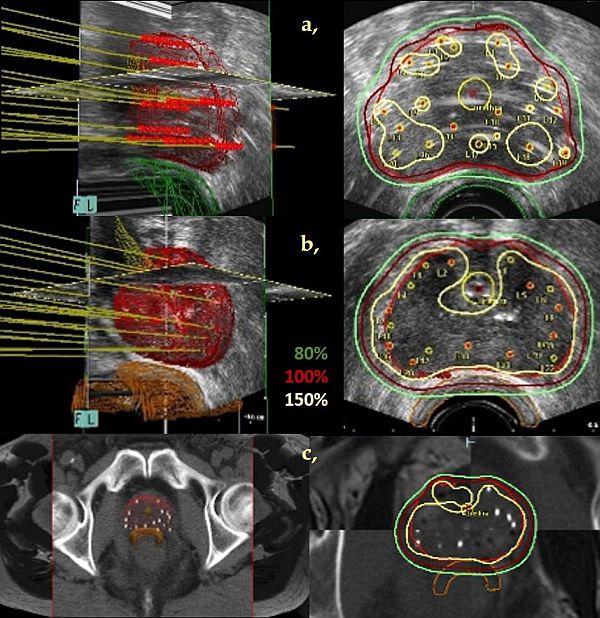
Figure. 3D reconstruction (left) and an axial TRUS or CT/MRI slice (right) of interstitial high-dose-rate (a,) and low-dose-rate prostate brachytherapy (live (b,) and postimplant (c,) ) plan. Red: prostate, yellow: prostatic urethra, brown: rectum wall.
Statistical comparisons with Mann-Whitney U-test were performed between the corresponding dose-volume parameters of HDR vs. LDR plans. Wilcoxon-matched pairs test was used in the comparison of live and postimplant plans of LDR BT.
Results
The mean prostate volume was 39.9 cm3, 35.6 cm3 and 36.2 cm3 in HDR, LDR live and postimplant plans. The median number of needles was 18 and 22, respectively. The V100 and V150 were 98.0% and 31.8% in HDR, whereas 98.9% and 60.4% in LDR live plans, and 89.7% and 52.1% in LDR postimplant plans. The dose distributions were more homogeneous and conformal with HDR technique, DHI was 0.68 vs. 0.39, COIN was 0.79 vs. 0.68. 4 weeks after the LDR implantation, the DHI increased to 0.42, the COIN decreased to 0.65 in postimplant plans. The urethra and rectum received significantly less dose with HDR BT. The D10 and D30 for urethra were 114.6% and 111.4%, respectively, in HDR, 134.4% and 129.0% in live and 139.4% and 142.0% in postimplant plans of LDR treatments. The D0.1 and D2 for rectum was 77.8 and 58.2% in HDR, 105.1% and 71.2% in live and 121.8% and 67.4% in postimplant plans of LDR BT, respectively (Table).
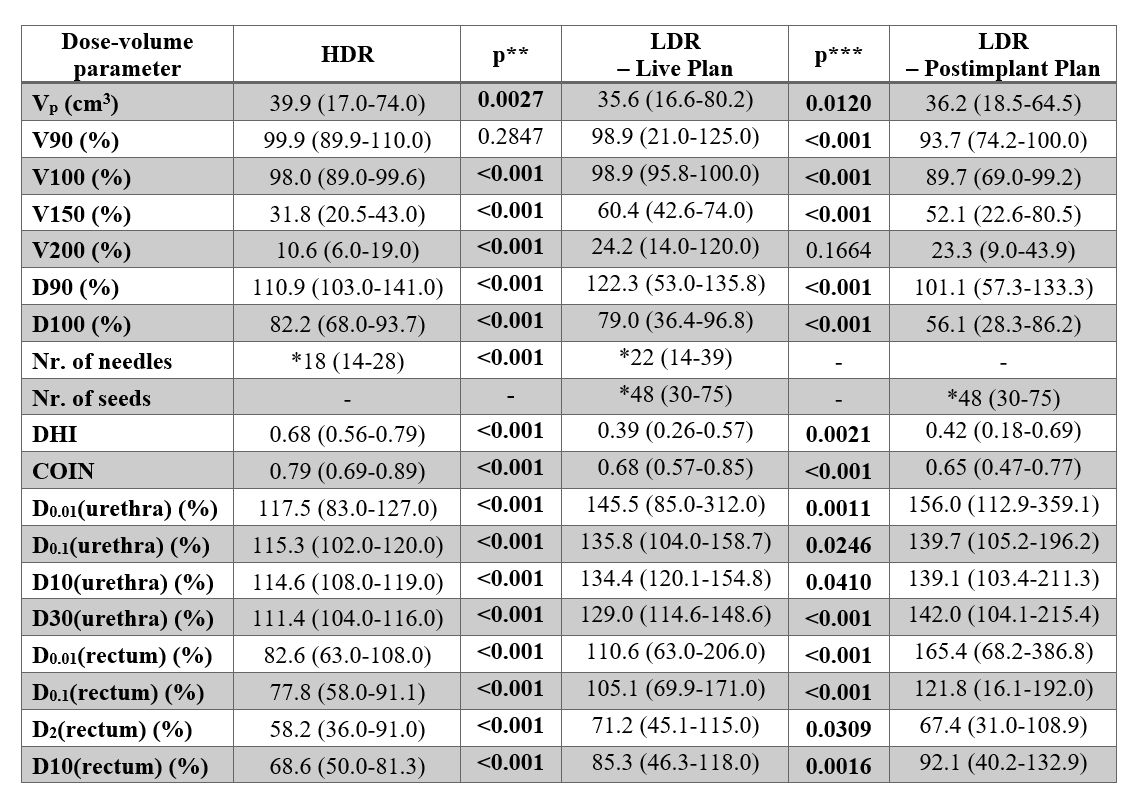
Table. Dose-volume parameters of single fraction high-dose-rate (HDR) and low-dose-rate (LDR) brachytherapy of prostate cancer. *Median. **Mann-Whitney-U Test. ***Wilcoxon Matched Pairs Test.
Conclusion
Both techniques provided acceptable target volume coverage. However, in plans 4 weeks after LDR implantation 5-10% poorer dose-volume parameters were observed, except for dose homogeneity. The dose distributions were more homogeneous and conformal, and both urethra and rectum were better protected with the HDR technique.