Organ positional differences between planning US and implant procedure in two-step LDR brachytherapy
Orla Houlihan,
United Kingdom
PO-2193
Abstract
Organ positional differences between planning US and implant procedure in two-step LDR brachytherapy
Authors: Orla Houlihan1,2, Sergio Esteve3, Owen McLaughlin3,2, Geraldine Workman3, Monica Byrne3, Kevin Prise2, Alan Hounsell3, Darren Mitchell1, Suneil Jain1,2
1Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Clinical Oncology, Belfast, United Kingdom; 2Queen’s University Belfast, Patrick G. Johnston Centre for Cancer Research, Belfast, United Kingdom; 3Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Radiotherapy Medical Physics, Belfast, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To quantify dosimetric differences for the prostate, urethra and rectum between the planning transrectal ultrasound (TRUS) and the implant procedure in two-step LDR brachytherapy.
Material and Methods
A TRUS was performed immediately prior to radioactive seed implantation for 25 patients undergoing two-step LDR prostate brachytherapy. The brachytherapy plan, generated from a planning TRUS performed 3-4 weeks prior to the implant procedure was imported onto this pre-implant TRUS. The prostate, urethra and rectum were contoured and the doses to these organs were compared to the dose received on the original planning TRUS. Institutional dose constraints were prostate V150% (volume receiving at least 150% of the prescription dose) < 60% and V200% < 20%, urethra D5% (minimum dose to the most irradiated 5%) < 150% and D30% < 130% and rectum D1cc (minimum dose to the most irradiated 1cc) < 100% and D0.1cc < 138%. Target coverage for prostate was D90% > 121% and V100% > 99.5%. Due to the small of the urethra, the dose to the percentage volume parameter is sensitive to the volume contoured (e.g. if extra slices are contoured cranially or caudally due to slice resolution). To mitigate this limitation, the absolute urethral volumes (in cm3) corresponding to 5% and 30% were initially extracted from the planning TRUS DVH. These absolute volumes were then interpolated on the DVH for the pre-implant TRUS. This method was independent of urethral volume contoured and therefore allowed direct comparison of these parameters.
Results
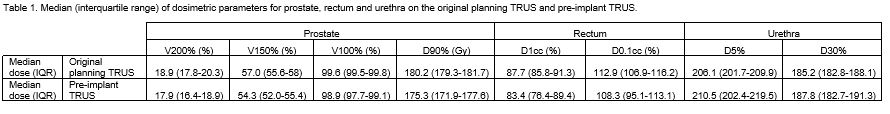
The median urethra D5% was greater on the pre-implant TRUS relative to the planning TRUS by 2.1% ((D5% pre-implant–D5% original)/(D5% original)*100) and the median urethra D30% was greater by 1.4%. The median rectum D1cc was lower by 4.9% and D0.1cc by 4.1% on pre-implant TRUS relative to the planning TRUS. The median prostate dosimetric parameters were also lower on the pre-implant TRUS compared to the planning TRUS with median differences relative to the planning TRUS for D90% of 2.8%, V100% of 0.7%, V150% of 4.7% and V200% of 5.3% (Table 1).
Using the DVH absolute volume interpolation method the number of cases exceeding dose constraints for urethra D5% increased from one on the original planning US to nine on the pre-implant TRUS, for urethra D30% increased from three on the original TRUS to fifteen on the pre-implant TRUS and for rectum D1cc and D0.1cc increased from zero on the original TRUS to one on the pre-implant TRUS. The urethral doses on the clinical plans were all within tolerance.
Conclusion
Median relative differences between the pre-implant TRUS and planning TRUS were low at ≤ 5.3% which is reassuring for centres performing two-step LDR prostate brachytherapy. The increased number of cases exceeding dose constraints for the urethra on pre-implant US may be a result of positional differences caused by relaxation of the urethra due to spinal anaesthetic used during the implant procedure and should be considered intra-operatively by the brachytherapy clinician.