Respiratory gated proton therapy for liver cancer: Setup accuracy and respiratory motion variabilty
PO-1962
Abstract
Respiratory gated proton therapy for liver cancer: Setup accuracy and respiratory motion variabilty
Authors: Esben Worm1, Saber Nankali2, Jakob Borup Thomsen2, Line Stick2, Morten Høyer2, Britta Weber2, Hanna Rahbek Mortensen2, Per Rugaard Poulsen2
1Aarhus University Hospital, Oncology, Aarhus, Denmark; 2Aarhus University Hospital, Danish Centre for Particle Therapy, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate (1) the accuracy of CBCT match to the exhale position of implanted fiducial markers in respiratory gated proton therapy for liver cancer and (2) the target motion variability between planning 4DCT and respiratory gated treatment fractions.
Material and Methods
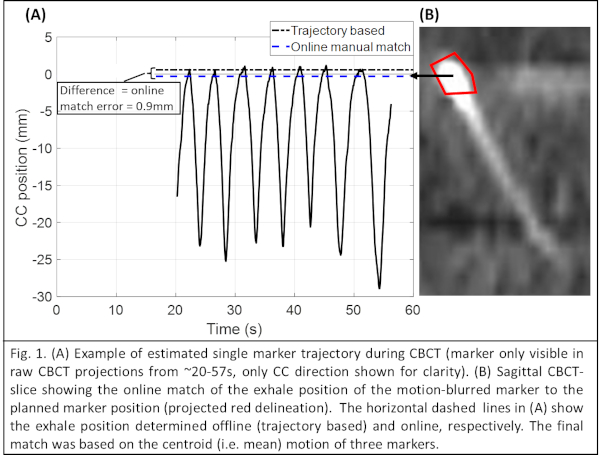
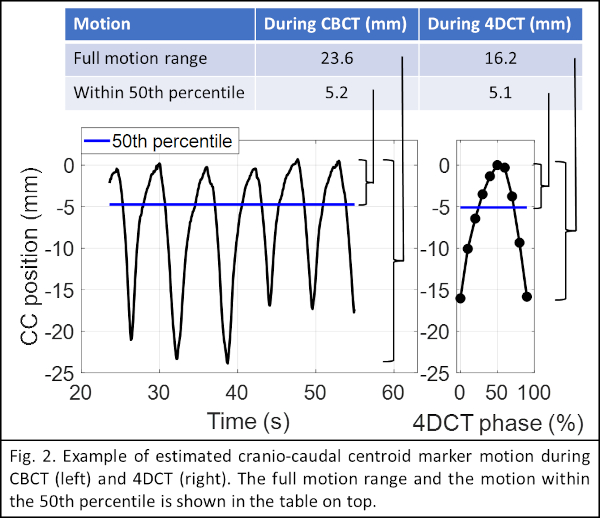
Four patients were treated with gated proton therapy with doses of 58 GyRBE or 67.5 GyRBE in 15 fractions. This study includes the planning 4DCT and CBCTs from the first 1-5 fractions of each patient (16 CBCTs). Planning was based on the exhale phase of a 10-phase 4DCT. An iCTV was formed as the union of the CTV in the 5 phases closest to exhale phase, corresponding to exhale respiratory gating with ~50% duty cycle. Robust SFUD optimization was performed with ±5mm (LR/AP) and ±7mm (CC) shifts and ±4.5% range uncertainty. Setup at each fraction was based on a free-breathing CBCT with manual match of the motion-blurred exhale position of three implanted fiducial markers (Fig. 1B). To investigate the match accuracy, the markers were retrospectively segmented in each raw 2D CBCT-projection (~1000 images per CBCT) and the time resolved 3D motion trajectory of the marker centroid during CBCT was estimated by a probability-based method. The exhale centroid position was defined as the 95th percentile position along the trajectory in each direction. The difference between this position and the online match defined the online match error (Fig.1A). To investigate motion variability, the marker centroid motion in 4DCT was compared with the estimated centroid motion during the CBCTs. Full motion ranges and motion within the 50th percentile (corresponding to the iCTV expansion and 50% duty cycle gating window) were determined (Fig. 2).
Results
The mean (±SD) online marker match error was -0.5±0.5mm (LR), 0.7±1.1mm (CC), -0.1±0.5mm (AP). Although the full motion range was considerably larger in CBCTs than in 4DCT (CC range 9.8mm larger), the motion ranges were very similar within the 50th percentile around full exhale (See table and Fig. 2).
| LR (mm) | CC (mm) | AP (mm) |
Mean (±SD) motion range during 4DCT and CBCT |
|
|
|
| Full motion 4DCT | 2.0±1.3
| 11.0±3.7
| 4.6±3.1
|
| Full motion CBCT | 3.6±1.8
| 21.5±4.1
| 10.6±5.5
|
| Within 50th percentile 4DCT | 0.7±0.4
| 4.0±1.4
| 1.8±1.4
|
| Within 50th percentile CBCT | 1.1±0.6
| 4.9 ±1.4
| 2.5±1.5
|
Mean (± SD) difference between motion range during 4DCT and CBCT
|
|
|
|
Difference of full motion
| 1.5±0.9
| 9.8±2.8
| 5.4±3.0
|
Difference within 50th percentile
| 0.4±0.4
| 0.4±1.6
| 0.4±0.9
|
Conclusion
Manual CBCT match to exhale marker position is prone to uncertainty, but acceptable errors close to the CT-resolution (~1mm LR/AP, 2mm CC) were observed. Large variations between the full motion in the planning 4DCT (one respiratory cycle) and during CBCT (several cycles) at treatment were observed. Respiratory exhale gating effectively limits both motion and motion variability and improves consistency between target volumes generated from 4DCTs (e.g. iCTVs/ITVs) and actual motion during treatment. More patients will be included in this study as they are treated.