Balancing Robustness and Adaptation for Proton Therapy of Lung Cancer Patients
PO-1945
Abstract
Balancing Robustness and Adaptation for Proton Therapy of Lung Cancer Patients
Authors: Vlad Badiu1,2, Vicki T. Taasti3, Wouter van Elmpt3, Edmond Sterpin1,4
1KU Leuven, Department of Oncology, Laboratory of Experimental Radiotherapy, Leuven, Belgium; 2UZ Leuven, Particle Therapy Interuniversity Center Leuven – PARTICLE, Leuven, Belgium; 3Maastricht University Medical Centre+, Department of Radiation Oncology (Maastro), GROW School for Oncology, Maastricht, The Netherlands; 4Université catholique de Louvain, Institut de Recherche Expérimentale et Clinique, Center of Molecular Imaging, Radiotherapy and Oncology (MIRO), Brussels, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
In proton therapy, robust planning is essential for accurate delivery in the presence of uncertainties. An increase in plan robustness leads to larger volumes irradiated with therapeutic doses and consequently a higher dose to adjacent organs-at-risk (OARs) and an increased chance of potential post-treatment toxicities. The opposite occurs with plans with a higher dose conformity to the target and subsequently sparing of healthy surrounding tissue at the expense of a higher sensitivity to anatomical changes, resulting in work and cost demanding adaptations. In this study we aim to identify the optimal workflow where the adaptation rate and the associated increase in upfront costs is balanced against dosimetric parameters or the potential post treatment detriment to the patient’s quality of life in the form of unwanted toxicities.
Material and Methods
Ten lung cancer patients were planned. Each patient had a planning CT and up to eight weekly repeated CTs (reCTs). Plans were made with three different levels of robustness with a setup error of 3, 6 or 9 mm, all with a range uncertainty of 2.6%. For each robustness level the planning dose was recomputed on all reCTs to assess whether the clinical constraints (e.g., target coverage and OAR dose) were met or if adaptation was required. Following the evaluation of dose metrics, we report the adaptation rate based on D98% nominal and worst-case values for target coverage as well as Dmean and V30% for heart and lungs-GTV and D2% for spinal cord and esophagus.
Results
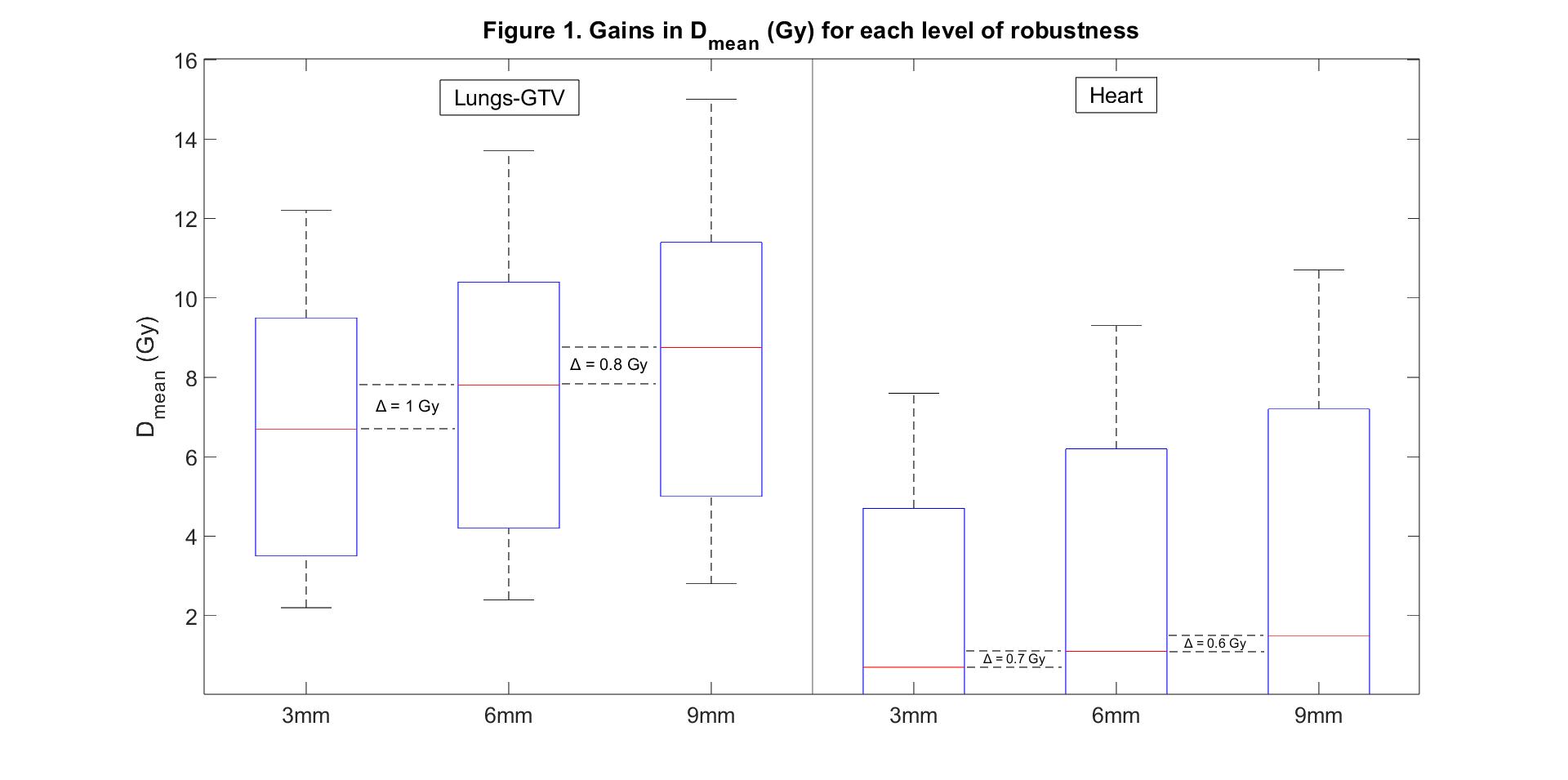
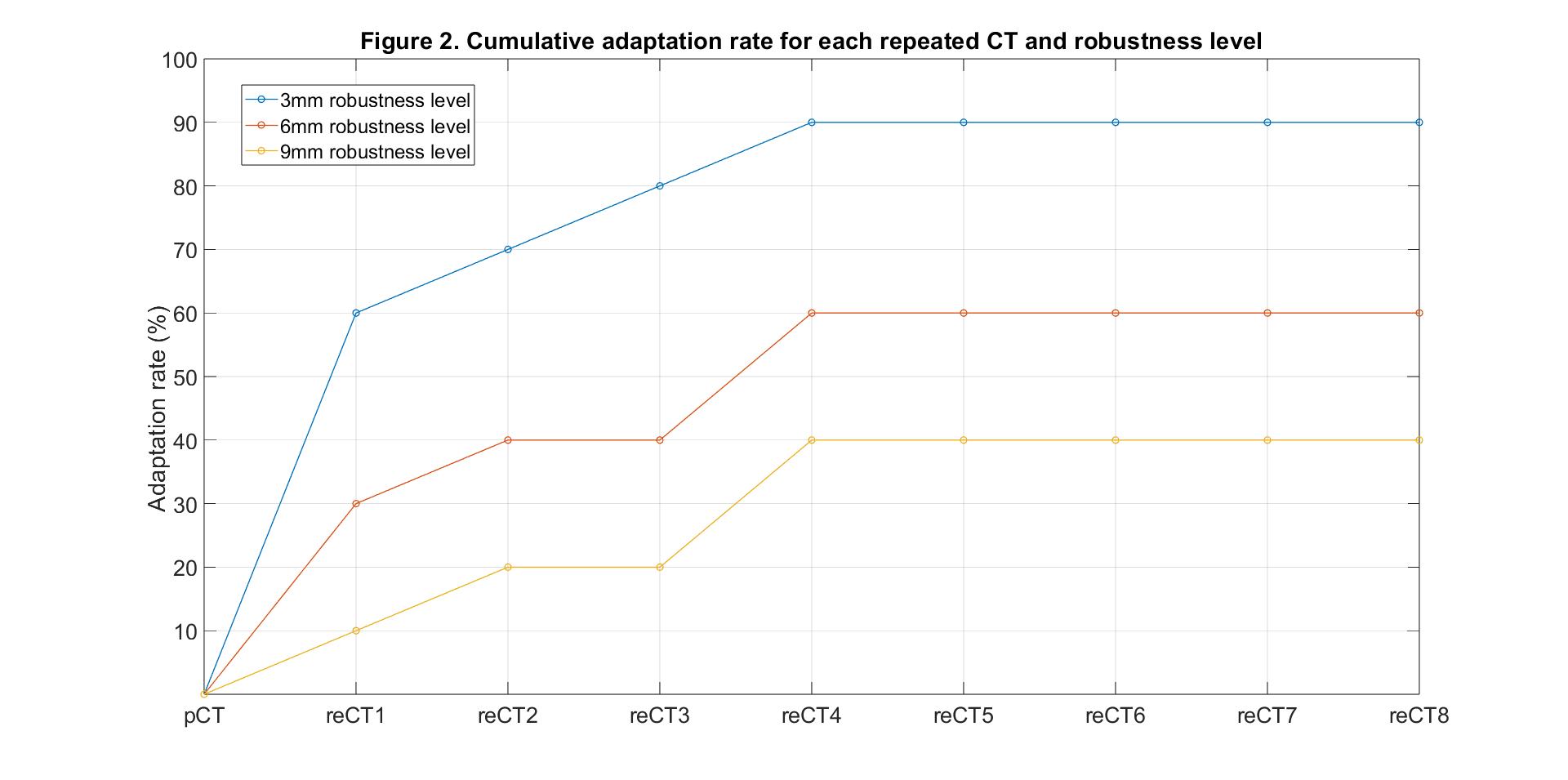
For the 3, 6 and 9 mm robustness levels, an adaptation rate of 90%, 60% and 40%, respectively, was observed. From these patients 78%, 83% and 50% needed an adaptation already within the first two weeks of treatment. This was expected, as an increase in robustness will decrease the susceptibility to anatomical changes. Average gains in OAR dose sparing were recorded when transitioning from a 9 mm setup error to 6 mm (lungs-GTV – 0.8 Gy Dmean, 1.2% V30%, heart – 0.6 Gy Dmean, 1.0% V30%, spinal cord – 2 Gy D2%, esophagus – 2.5 Gy D2%) and when transitioning from a 6 mm setup error to 3 mm (lungs-GTV – 1 Gy Dmean, 1.6% V30%, heart – 0.7 Gy Dmean, 1.0% V30%, spinal cord – 1.9 Gy D2%, esophagus – 2.9 Gy D2%). The gains for Dmean for Lungs-GTV and Heart are shown in Figure 1 as well as the weekly cumulative adaptation rate shown in Figure 2.
Conclusion
The expected increase in the adaptation rate at lower robustness levels and the benefit to the patient in the form of a reduced dose to OARs was confirmed in this study. In this way the most cost-effective trade-off workflow between plan robustness and the adaptation rate for proton therapy of lung cancer patients can be identified. The achieved OAR sparing can have significant clinical benefits in cases where lower robustness levels suffice for ensuring target coverage. This work also allows the identification of the optimal time point for adaptive treatment.